trihexyphenidyl FDA Approval
When working with trihexyphenidyl FDA approval, the official clearance of the anticholinergic drug trihexyphenidyl by the U.S. Food and Drug Administration, also known as Artane, it marks a key step for patients with Parkinson’s disease and certain movement disorders. The approval means the agency has judged the drug’s benefits to outweigh its risks based on clinical trial data. That judgment rests on three core pillars: safety, efficacy, and manufacturing quality. In plain terms, the FDA reviewed how the drug works, who it helps, and how consistently it can be produced.
Understanding the backdrop helps you see why this approval matters. anticholinergic medication, a class of drugs that block acetylcholine receptors to reduce muscle tremor and rigidity has been around for decades, but each new product still needs a fresh safety check. Trihexyphenidyl belongs to that class and is primarily prescribed for Parkinson's disease, a neurodegenerative disorder characterized by tremor, stiffness, and slowed movement. The drug’s ability to smooth out those motor symptoms makes it a valuable tool, especially for younger patients whose tremor is a major concern.
The FDA drug approval process, a regulated sequence of preclinical studies, Phase I‑III clinical trials, and comprehensive review is what turns a promising molecule into a marketable medicine. The process requires the sponsor to submit an NDA (New Drug Application) that includes detailed data on pharmacology, toxicology, dosing, and labeling. The agency then evaluates the data, often consulting advisory committees. Only after a positive assessment does the drug receive its official label and marketing rights. This pathway ensures that each approved medication meets a high standard of scientific rigor.
The approval also cleared several dosage forms, offering flexibility for patients and clinicians. Immediate‑release tablets are the most common, but extended‑release formulations exist for those who need steadier blood levels. Dosage adjustments are guided by patient age, kidney function, and severity of symptoms. Starting doses are typically low to gauge tolerance, and physicians may gradually increase the amount based on response. This titration strategy helps minimize side effects such as dry mouth, blurred vision, and constipation, which are common across anticholinergic drugs.
Why does all this technical detail matter to you? First, it tells you that trihexyphenidyl has passed a thorough vetting—so you can trust its risk‑benefit profile. Second, it highlights the drug’s place within a broader therapeutic class, helping you compare it to alternatives like benztropine or newer dopaminergic agents. Finally, knowing the approval timeline and required documentation equips you to ask the right questions when you talk to your healthcare provider.
The trihexyphenidyl FDA approval process set a benchmark for similar drugs, showing how safety data, efficacy outcomes, and manufacturing standards intersect. As you explore the articles below, you’ll find deeper dives on topics like drug interactions, patient counseling tips, and real‑world dosing experiences. This collection is designed to give you a practical roadmap, whether you’re a patient, caregiver, or healthcare professional seeking up‑to‑date information on this essential medication.
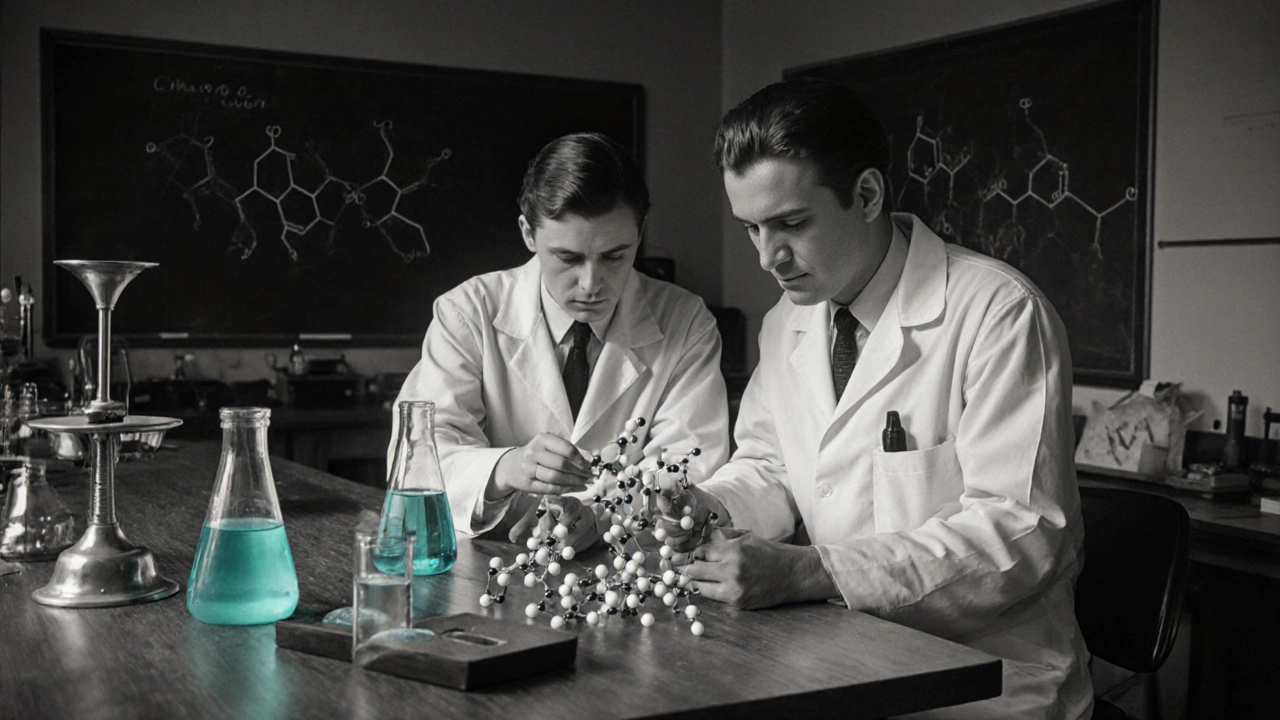
Trihexyphenidyl History: From 1950s Discovery to Modern Medical Use
Explore the full journey of trihexyphenidyl-from its 1950s discovery at Roche, FDA approval, clinical uses, side‑effects, and modern research-packed with timelines, comparisons, and FAQs.
read more