
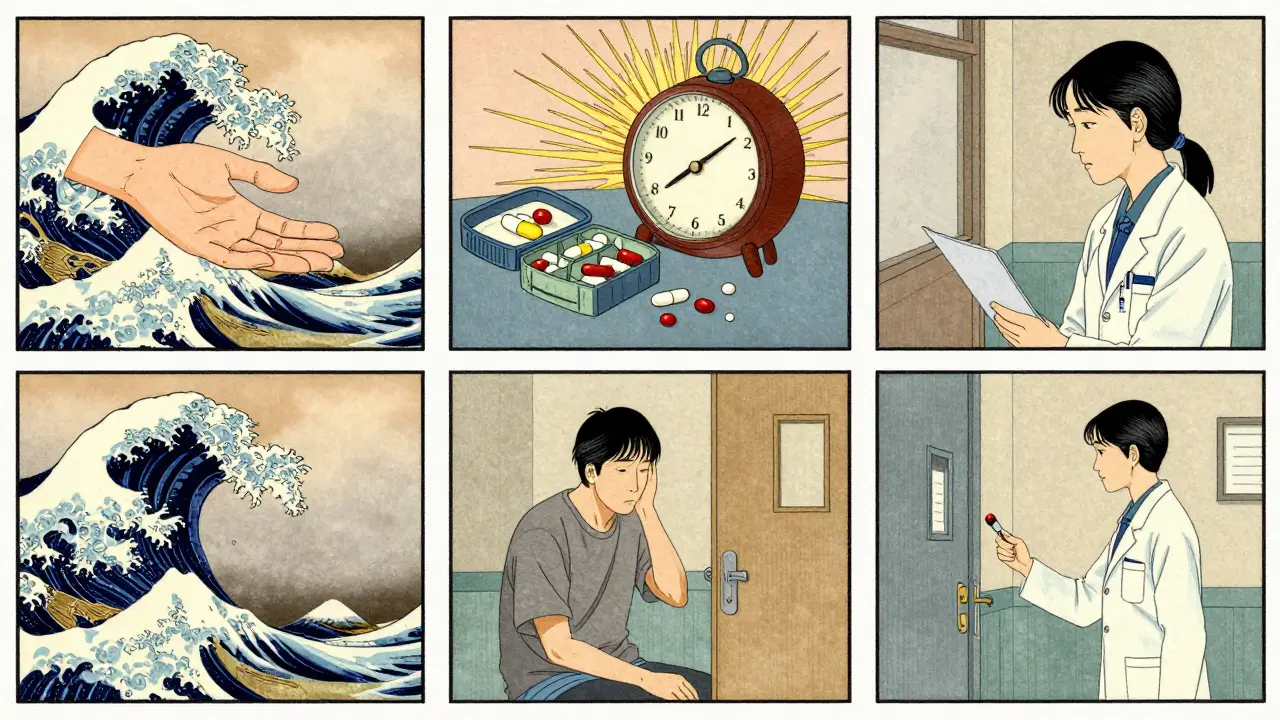
Imagine you’re prescribed a pill to lower your blood pressure. Your doctor tells you to take it every morning. You do it for a week, then skip a few days because you felt fine. A month later, you end up in the hospital. Was this your fault? Or was the system set up to fail you?
This isn’t just about forgetting a pill. It’s about how we talk about it. For decades, doctors and nurses called this compliance-as if patients were machines that needed to be programmed. But today, that language is outdated. And the shift from compliance to medication adherence isn’t just semantics-it’s saving lives.
What’s the Difference Between Adherence and Compliance?
At first glance, they sound the same. Take your medicine. Don’t miss doses. But the difference is deeper than wording.
Compliance means doing exactly what you’re told. No questions. No input. It’s a one-way street: doctor gives order, patient follows. If you don’t, you’re labeled non-compliant-as if you’re being disobedient.
Adherence is different. It’s about you, the patient, making an active choice to follow your treatment plan. It recognizes that you’re not a passive recipient-you’re a partner. You might skip a dose because the pill made you dizzy, or you can’t afford it, or you don’t believe it’s helping. Adherence doesn’t blame you. It asks: Why?
The American Pharmacists Association defines adherence as “the extent to which a patient’s behavior corresponds with agreed-upon recommendations.” Notice the word agreed-upon. That’s the key. It’s not about obedience. It’s about collaboration.
The shift started in the 1990s. Medical journals like the Journal of Clinical Pharmacy and Therapeutics and the Annals of Internal Medicine began pushing for this change. By the early 2000s, major health organizations had officially moved away from “compliance.” Today, the FDA, EMA, and WHO all use “adherence” in their guidelines. Even insurance companies and hospitals now track adherence-not compliance.
Why Does This Language Matter?
Words shape behavior. When you say “compliance,” you imply failure is personal. “You didn’t take your pills.” “You’re not following instructions.” That makes patients feel guilty, ashamed, or even rebellious.
When you say “adherence,” you open the door to understanding. “What got in the way?” “How can we fix this?”
Think about it: if you’re diabetic and your insulin costs $400 a month, and you’re working two jobs just to keep the lights on, are you “non-compliant” for skipping doses? Or are you making a rational decision under pressure? Adherence sees the system. Compliance only sees the person.
Studies show patients who feel heard are 2.57 times more likely to stick with their treatment. That’s not magic. It’s respect.
How Is Adherence Measured?
Adherence isn’t just a feeling. It’s measured. And the standards are clear.
The American Medical Association says you’re considered adherent if you take at least 80% of your prescribed medication. That’s it. Not 100%. Not perfect. Just 80%. Why? Because life happens. You forget. You travel. You feel better and think you don’t need it anymore.
Here’s how it’s tracked:
- Pill counts - Pharmacists count how many pills are left.
- Electronic monitoring - Smart caps on pill bottles record when they’re opened (called MEMS).
- Prescription refill records - Did you refill your statin on time?
- Self-reports - Simple questions: “How often do you miss doses?”
But here’s the catch: adherence isn’t just about taking the pill. It’s about three stages:
- Initiation - Did you start the medicine at all?
- Implementation - Are you taking it correctly, at the right time and dose?
- Discontinuation - Did you stop early, and why?
Compliance only looks at step two. Adherence looks at all three. That’s why it’s more accurate-and more helpful.
Where Does Compliance Still Show Up?
It’s not gone. It’s just limited.
In tuberculosis treatment, for example, nurses still watch patients swallow every pill. That’s called directly observed therapy (DOT). It works because TB is contagious and deadly-there’s no room for error.
But for chronic conditions like high blood pressure, diabetes, or depression? Compliance falls apart. Why? Because those conditions don’t have immediate symptoms. You don’t feel sick when you skip a dose. So you stop. And then you end up in the ER.
According to the World Health Organization, 50% of patients stop taking their long-term medications within the first year. That’s not laziness. That’s a system that doesn’t listen.
What Works Better: Adherence-Focused Care
Health systems that switch to adherence-focused care see real results.
A 2022 study by the National Community Pharmacists Association found that clinics using motivational interviewing-where providers ask open-ended questions like “What’s been hard about taking your meds?”-saw a 37.6% increase in adherence.
Tools like Hero Health and Dose Packer help too. One Kaiser Permanente trial showed a 42% drop in missed doses after using a smart pill dispenser that sends reminders and tracks usage. Another trial across 12,000 patients improved medication possession ratios by nearly 29%.
And it’s not just tech. It’s training. Providers now need 8-12 hours of special training to learn how to talk about meds without sounding judgmental. Electronic health records now flag patients at risk of non-adherence so pharmacists can reach out before they crash.
The Agency for Healthcare Research and Quality calls adherence “a cornerstone of effective chronic disease management.” And they’re right. Patients in adherence-focused programs have 20-50% higher treatment success rates.
The Business Side: Why Hospitals Care
This isn’t just about kindness. It’s about money.
When patients don’t take their meds, they end up in the hospital. And hospitals pay for that.
Since January 2024, the Centers for Medicare & Medicaid Services (CMS) has tied 8% of hospital payments to medication adherence rates for heart failure, COPD, and other chronic conditions. Miss the target? You lose money.
That’s why 87% of major U.S. health systems switched to adherence language by mid-2024. Even insurance companies now offer discounts for patients who use adherence apps.
The global market for adherence tools hit $4.2 billion in 2023 and is expected to hit $11.7 billion by 2028. Meanwhile, compliance-focused products? They’re fading. Less than 15% of new healthcare contracts now use compliance terminology.
What’s Next? AI and the Future of Adherence
The future is personal.
Google Health’s 2024 study used machine learning to predict who would miss doses-not by looking at medical history, but by analyzing 27 factors: income, transportation, sleep patterns, even social media activity. The system predicted adherence with 83.7% accuracy.
And in 2025, the American Medical Association added new billing codes (99487-99489) specifically for adherence counseling. That means doctors can now get paid for talking to patients about their meds-really talking-not just handing out prescriptions.
The WHO projects that if adherence-focused care becomes universal, it could prevent 850,000 premature deaths annually in low- and middle-income countries by 2030. That’s not a guess. That’s data.
What You Can Do
If you’re a patient:
- Ask: “What happens if I don’t take this?”
- Speak up if side effects are bad or it’s too expensive.
- Use a pill organizer or phone reminders.
- Don’t stop meds just because you feel better-talk to your provider first.
If you’re a caregiver or family member:
- Don’t nag. Ask: “What’s making it hard?”
- Help them set up refill reminders.
- Go with them to appointments if they’re overwhelmed.
If you’re a provider:
- Stop saying “compliance.” Say “adherence.”
- Use motivational interviewing: “Tell me about your routine.”
- Check in on cost barriers-many patients won’t say it unless you ask.
- Use EHR alerts to flag at-risk patients.
Final Thought
Medication adherence isn’t about perfection. It’s about partnership. It’s about recognizing that people aren’t problems to be fixed-they’re people with lives, fears, and real barriers.
The old way blamed the patient. The new way asks: What do we need to change to help them succeed?
That’s not just better medicine. It’s more human.
Is medication adherence the same as compliance?
No. Compliance means following orders without question. Adherence means actively choosing to follow a treatment plan based on mutual understanding and agreement with your provider. Adherence recognizes your reasons for missing doses-like cost, side effects, or forgetfulness-and works with you to solve them. Compliance just labels you as non-compliant.
What percentage of medication use counts as adherence?
According to the American Medical Association, you’re considered adherent if you take at least 80% of your prescribed medication over a given period. This accounts for real-life factors like occasional missed doses, travel, or side effects. It’s not about perfection-it’s about consistency.
Why do people stop taking their medications?
There are many reasons. The most common include: side effects, high cost, feeling better and thinking it’s no longer needed, complex dosing schedules, forgetfulness, or cultural beliefs about medicine. Many patients don’t tell their doctors because they fear being judged. Adherence-focused care asks these questions without blame.
Can technology help with medication adherence?
Yes. Smart pill dispensers, phone apps, and electronic monitoring caps (like MEMS) can track when doses are taken and send reminders. Studies show tools like Hero Health and Dose Packer reduce missed doses by 28-42%. AI is also being used to predict who’s at risk of non-adherence based on lifestyle, income, and behavior patterns.
Are doctors trained to support medication adherence?
More than ever. Since 2023, many health systems require providers to complete 8-12 hours of training in communication techniques like motivational interviewing. New CPT billing codes (99487-99489) now pay doctors for spending time talking with patients about their meds-not just prescribing them.
Is adherence used in all healthcare settings?
Mostly, yes. By 2024, 87% of major U.S. health systems had adopted adherence-focused language and protocols. However, some settings like correctional facilities still use compliance language-63% of them, according to the National Commission on Correctional Health Care. But even there, pressure is growing to change.
What’s the biggest benefit of adherence over compliance?
The biggest benefit is improved outcomes with less blame. Adherence reduces hospital readmissions by 22-34% and cuts treatment costs by 18-27%. More importantly, it builds trust. Patients who feel heard are far more likely to stick with their treatment long-term-not because they’re forced to, but because they want to.
Okay but let’s be real - if your doctor can’t even spell 'adherence' correctly on the prescription, why should I trust them to manage my health? I’ve been told to 'just take it' for years. Now they wanna rebrand it? Cool. But I’m still paying $600 for a 30-day supply of blood pressure meds. Call it what you want - it’s still a luxury.
They’re rewriting history to make the system look better. Compliance wasn’t bad - it kept people alive. Now we’re all supposed to be 'partners'? Please. The FDA, WHO, and big pharma pushed this shift because they don’t want to fix the real problem: drug prices. They’d rather guilt-trip patients than lower costs. This is corporate PR dressed up as empathy.
I think this is actually huge but nobody talks about the third stage enough
Like yeah we get initiation and implementation but discontinuation is where the system totally drops the ball
People stop because they feel stupid asking about side effects or because their doctor looks at them like they’re wasting time
And then they just vanish from the system
And nobody checks in
And that’s not adherence failure
That’s care failure
Thank you for articulating this so clearly. The shift from compliance to adherence represents a fundamental evolution in patient-centered care. It acknowledges human complexity - not just biological factors, but socioeconomic, psychological, and logistical barriers. This is not semantics. It is a paradigm shift rooted in dignity. When providers are trained in motivational interviewing and empowered with tools like EHR alerts, outcomes improve - not because patients are 'better behaved,' but because they are seen. This is medicine at its best.
As someone who’s watched my mom struggle with diabetes for 15 years, I’ve seen both sides
She used to feel like a failure every time she missed a dose
Then her new nurse asked 'what’s the hardest part?'
Turns out she was skipping insulin because she didn’t want to eat alone
So now we eat dinner together every night
And her A1c dropped 2 points
It’s not about the pill
It’s about the person behind it
So we’re calling it 'adherence' now? Cute. Next they’ll rename 'obesity' to 'body diversity' and 'smoking' to 'nicotine engagement.'
People forget pills because they’re lazy. Call it what it is.
Did you know the WHO is funded by big pharma? They pushed 'adherence' so they could sell you smart pill dispensers and apps that track your every swallow
They want your data
They want your habits
They want to know when you skip a dose so they can upsell you a more expensive version
It’s not about care
It’s about control
And your doctor? They’re just the middleman
This hit me right in the feels 😔
My grandma took her meds religiously for 10 years… then stopped because she couldn’t afford the copay and didn’t want to tell anyone
She thought she was being 'strong'
Turns out she just needed someone to ask
Thanks for saying this
❤️
Too long didn't read. But I skip my meds sometimes. So yeah.
Let’s not sugarcoat this - this whole 'adherence' movement is a socialist fantasy wrapped in therapist jargon. You think asking 'what got in the way?' fixes the fact that people are choosing not to take their medicine? No. It just lets them off the hook. Discipline. Responsibility. Those aren’t outdated concepts - they’re the backbone of a functioning society. If you can’t follow a simple prescription, maybe you shouldn’t be trusted with a pill bottle. The system isn’t broken - your attitude is.