
Many people assume cochlear implants are only for those who are completely deaf. That’s not true anymore. If you’ve been struggling to understand conversations even with hearing aids-if you’re tired of asking people to repeat themselves, avoiding social events, or missing the sound of your grandchildren’s laughter-you might be a better candidate for a cochlear implant than you think.
It’s Not About How Much You Can Hear Anymore
The old rule was simple: if you couldn’t hear anything at all, you got a cochlear implant. But that thinking changed in 2023. New guidelines from the American Cochlear Implant Alliance now say: if you’re getting less than 50% of words right with properly fitted hearing aids, you should be evaluated. That’s it. No need to wait until you can’t hear speech at all.
Before, clinics used to require a pure-tone average of 70 dB or worse at key frequencies. Now, they look at how well you understand speech in real life. A person with moderate hearing loss but terrible word recognition might be a better candidate than someone with profound loss who still understands 60% of words. Why? Because the brain starts to forget how to process sound if it’s not getting clear input. The longer you wait, the harder it becomes to recover that ability-even after surgery.
That’s why experts now say: refer early. Even if you still hear some things, if you’re struggling, it’s time to talk to an audiologist who specializes in implants. There’s no such thing as a bad referral. Getting checked doesn’t mean you have to get the device-it just means you know your options.
What the Evaluation Actually Involves
The evaluation isn’t a single test. It’s a full picture of your hearing, your health, and your life. Most clinics will schedule you for three to four appointments over a few weeks.
First, they’ll check your hearing aids. Not just whether they’re turned on-but whether they’re actually working right for your ears. Many people are turned down because their hearing aids aren’t properly fitted. Real-ear measurements are used to confirm the devices are delivering sound exactly where they should. If your aids aren’t optimized, you’re not getting a fair shot at hearing.
Then comes speech testing. You’ll listen to lists of words like “cat,” “dog,” “ball” in a quiet room. You’ll repeat them. Then you’ll do the same with sentences like “The boy kicked the red ball.” The gold standard is the AzBio sentence test-it’s designed to mimic real conversations. If you score below 50%, you’re in the candidate range.
They’ll also test you in noise. Real life isn’t quiet. If you can understand speech in a quiet room but freeze up in a restaurant, that’s a red flag. They might use the Speech, Spatial and Qualities of Hearing Scale (SSQ) to measure how well you function in everyday situations-like knowing where someone is talking or understanding TV without subtitles.
After that, you’ll see an ear, nose, and throat specialist. They’ll look at your inner ear with a CT or MRI scan. They need to make sure your cochlea isn’t blocked, scarred, or malformed. Most people have no issues here, but if there’s a structural problem, it can affect how the implant works.
Finally, they’ll talk to you about motivation. Do you want to talk to family again? Can you commit to the follow-up appointments and rehab? Cochlear implants don’t work like magic. They need time, training, and patience. But if you’re ready to try, you’re already ahead of most people.
Who Gets Left Out-and Why That’s Changing
For years, people with single-sided deafness were told they didn’t qualify. Same with those who had hearing loss in one ear and normal hearing in the other. That’s changing. Now, if one ear is so bad it’s dragging you down, even if the other ear is fine, you can be a candidate.
That’s huge. About 8.3% of people with hearing loss have this kind of asymmetric loss. They often struggle with directionality-knowing where sounds come from-and in noisy places. Many of them don’t even realize their hearing aids aren’t helping because they’re relying on their good ear. A cochlear implant on the bad side can restore balance and make everything easier.
Age used to be a barrier too. People over 65 were often told it wasn’t worth it. But the data says otherwise. A 2021 study found that older adults implanted after 15 years of deafness had the same improvement in speech understanding as younger patients-so long as they were cognitively healthy and willing to do the rehab work.
Even people with long-standing hearing loss are now being considered. The old myth was: “If you’ve been deaf for 20 years, your brain won’t remember how to hear.” But brain imaging studies show that the auditory pathways stay alive longer than we thought. With the right stimulation, they can wake up.
What Happens After the Surgery
Surgery takes about two hours. It’s outpatient-you go home the same day. The device is turned on about three to four weeks later, once healing is complete.
That first activation is emotional. Some people hear beeps and chirps. Others hear voices clearly right away. It depends on how long your brain has been without clear sound. Most people need four to six months of regular rehab to get the most out of the device.
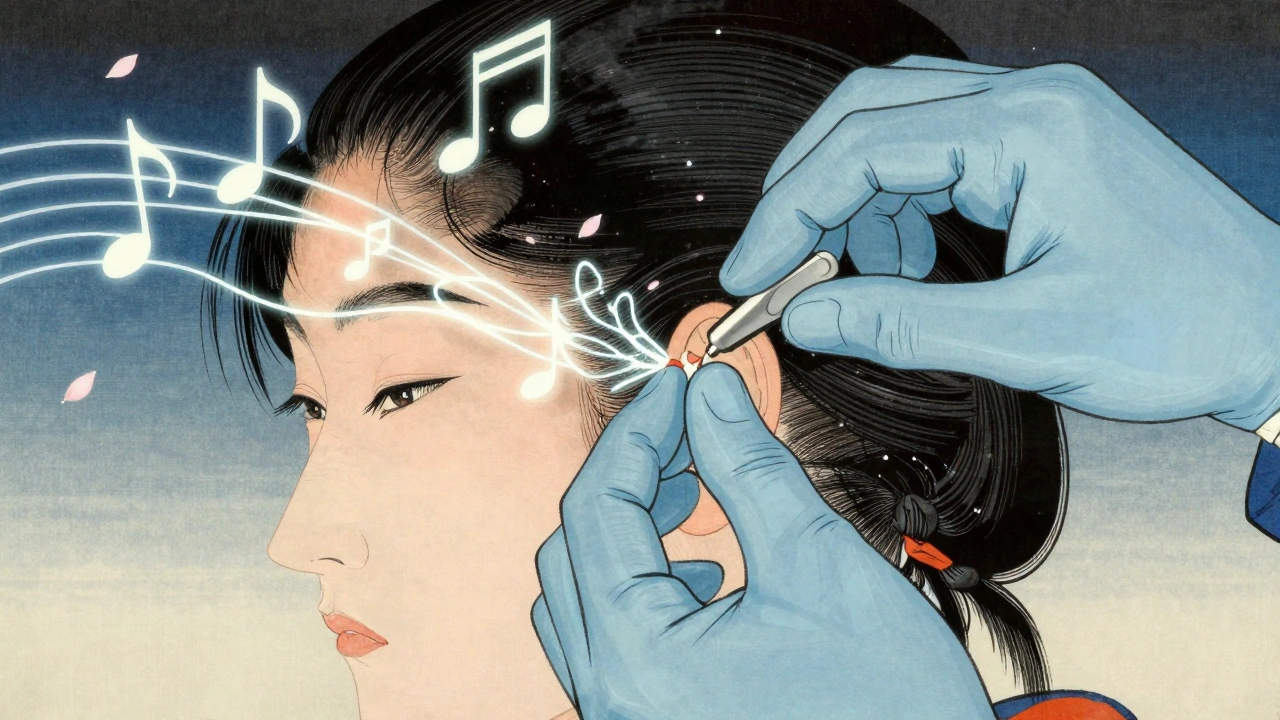
You’ll work with an audiologist to adjust the settings. The implant doesn’t restore normal hearing-it gives you a different kind of sound. Think of it like learning a new language. Your brain has to relearn how to interpret electrical signals as speech.
Most people see big improvements in quiet settings within three months. By six months, 89% report substantial improvement in daily communication. Phone calls become possible again. Watching TV without captions? That’s common. One patient said, “I heard my dog bark for the first time in 12 years. I cried.”
Music is still tricky. About 63% of users say they don’t enjoy music the way they used to. But many learn to appreciate rhythm and melody over time. Some even start playing instruments again.
The Real Results: Numbers That Matter
Let’s look at what the data says. A 2022 study of 1,247 adults found that those who met the new 50% word-recognition threshold improved their speech understanding by an average of 47 percentage points after implantation. That’s not a small gain-it’s life-changing.
In the ERID clinical trial, older adults who didn’t meet old Medicare criteria (but scored 40-60% with hearing aids) still had a 78% success rate post-implant. That means nearly 8 out of 10 people who were told “you’re not a candidate” actually benefited.
And it’s not just about hearing. People report less fatigue. Less anxiety. More confidence. One user on Reddit wrote: “I stopped canceling family dinners. I started going to church again. I didn’t realize how lonely I’d become.”
There are downsides. Some people have trouble with background noise. Others get headaches at first. But these usually improve with time and tuning. The risk of serious complications is less than 1%.

Why So Few People Get Them
There are an estimated 38 million American adults with disabling hearing loss. In 2022, only 128,000 cochlear implants were done. That’s less than 1%.
Why? Because most doctors don’t know the new guidelines. A 2021 survey found only 32% of primary care physicians could correctly identify who qualifies. Many still think you need to be totally deaf. Others assume hearing aids are enough. And patients? They don’t know to ask.
There’s also a stigma. Some people feel like implants are “extreme.” But they’re no more extreme than getting glasses for poor vision. Hearing loss is a medical condition. Cochlear implants are a proven, safe treatment.
Cost isn’t usually a barrier either. Medicare, Medicaid, and most private insurers cover the full cost of the device, surgery, and follow-up care. The real cost is in waiting-lost jobs, social isolation, increased risk of dementia.
Studies show cochlear implants give back three dollars for every dollar spent-through better employment, fewer doctor visits, and reduced cognitive decline. That’s not just a health win. It’s an economic one.
What Comes Next
The FDA is reviewing new labeling for all three major implant makers (Cochlear, Advanced Bionics, MED-EL) to reflect the 50% word-recognition threshold. By 2030, experts predict cochlear implants will be standard care for anyone with hearing loss over 55 dB and speech understanding below 60%-even if they still have some natural hearing.
Research is moving fast. Scientists are testing brainwave responses and inner ear signals to predict who will benefit most. Soon, we might be able to tell-not just from speech tests, but from biology-whether an implant will work.
But right now, the biggest barrier isn’t technology. It’s awareness. If you or someone you love is struggling to hear-even with hearing aids-it’s time to get evaluated. You don’t have to be perfect. You don’t have to be desperate. You just have to be ready to try.
Do I need to be completely deaf to get a cochlear implant?
No. You don’t need to be completely deaf. If you understand fewer than 50% of words with properly fitted hearing aids, you’re likely a candidate-even if you still hear some sounds. The goal is to stop waiting until it’s too late.
Can older adults benefit from cochlear implants?
Yes. Age doesn’t matter as much as brain health and willingness to participate in rehab. People over 65, even those with 15+ years of hearing loss, have shown the same level of improvement as younger patients when they follow through with therapy.
What if I only have hearing loss in one ear?
You can still qualify. Single-sided deafness is now a recognized indication. If one ear is so poor it’s making it hard to understand speech or locate sounds, an implant on that side can restore balance and significantly improve your ability to hear in noisy places.
Is the surgery risky?
It’s very safe. The risk of serious complications like facial nerve damage or infection is less than 1%. Most people go home the same day and return to normal activities within a week.
Will I hear normally after the implant?
You won’t hear exactly like you did before hearing loss. The implant gives you electrical signals that your brain learns to interpret as sound. Most people regain clear speech understanding in quiet settings. Music and noisy environments are harder, but many adapt over time.
How long does it take to see results?
Most people notice improvement within a few weeks. But it takes 3-6 months of consistent listening and rehab to reach your best performance. Patience and practice are key.
Are cochlear implants covered by insurance?
Yes. Medicare, Medicaid, and most private insurers cover the full cost of the device, surgery, and follow-up care. The only out-of-pocket expense might be a small copay for clinic visits.
What if I’m not a candidate? Is the evaluation still worth it?
Absolutely. Even if you don’t qualify for an implant, the evaluation gives you a full hearing profile. You might learn your hearing aids need reprogramming, or that you have a treatable medical issue. Either way, you’ll have a clear plan for your hearing health.
If you’ve been avoiding conversations because you can’t keep up, or if you’re tired of pretending you heard what someone said-don’t wait. Get evaluated. The best time to act wasn’t years ago. It’s now.
Man, this post hit different. I’ve had a cochlear implant for 3 years now and honestly? The first time I heard rain on the roof again, I just sat there like an idiot smiling. No joke. My wife thought I lost it. But you don’t realize how much silence weighs on you until it’s gone.
Also, music still sucks. But I can tell when my kid’s singing off-key now. That’s a win.
Look, if you’re still waiting for your hearing aids to ‘do the trick’ while you’re nodding along at dinner parties like a polite ghost-you’re not being patient, you’re being punished. This isn’t a luxury. It’s a reset button for your social life.
I’ve seen people come in with 15 years of deafness and walk out crying because they heard their grandkid say ‘I love you’ without shouting. Don’t wait until you’re too tired to care. Your brain’s still listening. It just needs a new signal.
I’m 68 and got mine last year. I didn’t know I was missing so much until I heard birds again. It’s not perfect. But it’s enough.
While the clinical data presented here is statistically robust, one must critically interrogate the epistemological framing of ‘speech understanding’ as the sole metric of auditory efficacy. The reductionist paradigm of quantifying human auditory experience via AzBio or SSQ scales neglects the phenomenological dimension of sound-the emotional resonance, the timbral nuance, the cultural context of sonic perception. One might argue that the normalization of cochlear implant candidacy under the 50% threshold reflects not a medical advancement, but a neoliberal commodification of auditory function, wherein the body is reconfigured as a problem to be optimized rather than a lived experience to be understood.
Furthermore, the assertion that ‘there’s no such thing as a bad referral’ assumes a homogenous patient subjectivity, ignoring socioeconomic disparities in access to audiological follow-up, linguistic diversity in speech testing materials, and the psychological toll of prolonged auditory deprivation. This is not progress. It’s protocol.
It is imperative to underscore that the clinical criteria outlined herein are consistent with the updated guidelines promulgated by the American Cochlear Implant Alliance (ACIA) as of Q3 2023, which supersede the prior thresholds established under CMS reimbursement protocols. The shift from pure-tone average to speech-in-noise recognition as the primary eligibility metric represents a paradigmatic evolution in audiological practice, aligning with evidence-based outcomes from longitudinal studies including the ERID cohort (2022) and the HARMONY trial (2021).
Moreover, the integration of real-ear measurements and cognitive screening protocols ensures that candidacy assessments are not merely audiometric but holistic. Clinicians are advised to document baseline SSQ scores, conduct CT/MRI evaluations for cochlear patency, and assess motivation via structured interviews prior to referral. Failure to adhere to this multi-modal framework may result in suboptimal outcomes and increased revision rates.
They make it sound easy. But try explaining to your family why you need surgery to hear them yell at you.
Let’s be real-the real reason implants are being pushed is because the hearing aid industry is losing billions. Why sell $3,000 devices that need new batteries every week when you can sell a $50K implant with a 10-year lifespan? The ‘50% word recognition’ threshold? That’s not medicine. That’s marketing.
And don’t get me started on the ‘music is still tricky’ disclaimer. If you can’t enjoy music after an implant, you’re not hearing-you’re processing data.
Interesting how we’ve reduced the sublime act of listening to a binary metric: ‘Can you repeat ‘cat’ or ‘dog’?’
But what of the silence between words? The pause before a laugh? The hum of a kettle that used to mean dinner was coming? We’re not just restoring hearing-we’re engineering compliance. The implant doesn’t bring back sound. It brings back productivity.
And yet… I still cried when I heard my daughter’s voice again. So maybe the system works, even if the logic doesn’t.
...And yet, the FDA hasn’t mandated long-term neuroplasticity studies. No one’s tracking how many people develop tinnitus post-implant. No one’s asking if the brain rewires itself into a state of chronic hyperstimulation. This isn’t medicine. It’s a beta test on human subjects. And we’re all just nodding along because ‘it’s better than nothing.’
Meanwhile, the implant companies are sponsoring every audiologist conference. Coincidence? I think not.
People like you think you’re helping but you’re just making deaf people feel guilty for not trying harder. My uncle has been deaf since 1970 and he’s happy. He reads lips, he signs, he lives. Why force him to get a metal chip in his head just so he can hear the TV louder? You’re not helping. You’re erasing culture.
wait so if i hear 49% of words with hearing aids im a candidate? what if i just dont care? what if i like quiet? why is everyone so desperate to hear everything? i dont get it
bro i got one last year and i still can't hear my wife when she's mad. the implant didn't fix my marriage. 😔
I work with older adults who’ve waited decades to get evaluated. Some of them come in with tears in their eyes because they finally feel like they’re not a burden. It’s not about the technology-it’s about dignity. Being able to hear your grandchild say ‘I love you’ without shouting across the room? That’s not a medical win. That’s a soul win.
If you’re hesitating because you think you’re ‘not bad enough’-you’re wrong. You’re not waiting for permission. You’re waiting for courage. And that courage? It’s already inside you. You just need to ask for help.
...And yet, the cochlear implant manufacturers are owned by the same conglomerates that control Big Pharma, the CDC, and the FDA. Did you know that the 50% threshold was introduced exactly 6 months after Cochlear Ltd. received a $2.1B government contract? Coincidence? Or is this a manufactured crisis to drive demand? The truth is buried under clinical jargon. Don’t let them tell you what’s ‘normal.’