Congestive Heart Failure: Signs, Causes, and Management
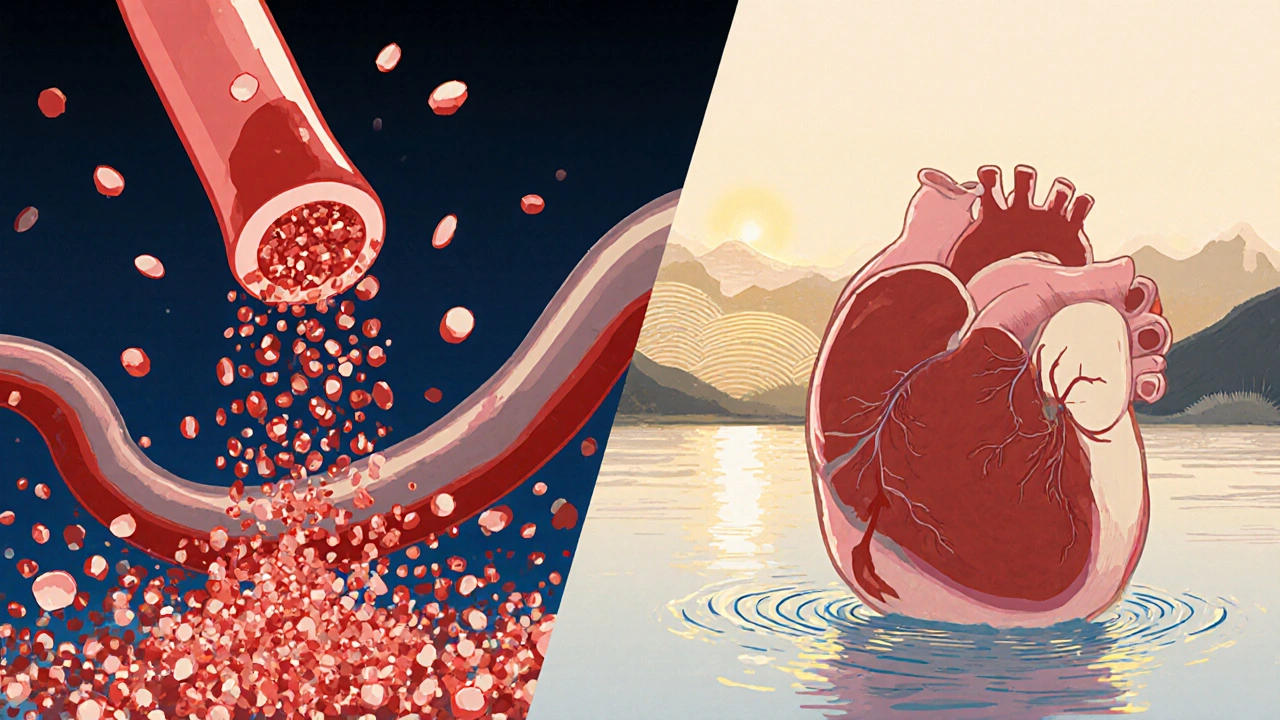
When dealing with congestive heart failure, a chronic condition where the heart cannot pump blood efficiently, leading to fluid buildup. Also known as CHF, it often involves fluid overload, excess fluid that collects in the lungs, abdomen, or legs and worsens heart strain. Recognizing these core concepts helps you see why everyday habits matter and why medical care focuses on removing that extra fluid.
People with congestive heart failure usually notice shortness of breath after mild activity, swelling in the ankles or belly, and persistent fatigue. The shortness of breath, often called dyspnea, happens because fluid leaks into the lung tissue, compromising oxygen exchange. Swelling, or edema, is the visible sign of fluid overload pushing into the lower extremities when gravity pulls the excess fluid down. Fatigue results from the heart’s reduced output, so the muscles receive less oxygen and energy. These symptoms often appear together, creating a cycle that can quickly degrade quality of life if not addressed.
Doctors confirm the condition using several tests, and one of the most telling numbers is the ejection fraction, the percentage of blood the left ventricle pumps out with each beat. An ejection fraction below 40% usually signals systolic dysfunction, while a reading closer to 55% or higher may indicate diastolic issues where the heart can’t relax properly. Blood tests for B-type natriuretic peptide (BNP) rise when the heart stretches, and imaging like echocardiograms shows the heart’s structure and motion. Together, these metrics paint a clear picture of how severe the fluid overload is and guide treatment choices.
Practical Treatment Strategies for CHF
Removing excess fluid is the first priority, and that’s where diuretics, medications that increase urine output to flush out extra fluid become essential. Loop diuretics such as furosemide act fast, while thiazide-type drugs help maintain balance over longer periods. Alongside meds, doctors prescribe ACE inhibitors or ARBs to relax blood vessels, beta‑blockers to reduce heart strain, and sometimes aldosterone antagonists for added fluid control. Lifestyle tweaks matter just as much: limiting sodium intake to less than 2,000 mg daily curbs water retention, and regular low‑impact exercise improves circulation without overtaxing the heart.
Self‑monitoring empowers patients to catch worsening fluid overload early. Weighing yourself every morning and noting a jump of more than two pounds signals that fluid is accumulating and may require a dose adjustment of diuretics. Keeping a symptom diary—recording breathlessness, swelling, and energy levels—helps clinicians fine‑tune treatment plans. Education on medication timing, recognizing side effects like low potassium, and knowing when to seek urgent care (e.g., sudden chest pain or severe shortness of breath) are all parts of a comprehensive care plan.
All these pieces—understanding fluid overload, tracking ejection fraction, using diuretics wisely, and adopting heart‑friendly habits—form a roadmap for living with congestive heart failure. Below, you’ll find a curated collection of articles that dive deeper into specific meds, lifestyle tips, and the latest research, giving you practical steps to manage the condition and improve daily life.
Diabetes and Congestive Heart Failure: How They’re Linked
Explore how diabetes fuels congestive heart failure, the shared risk factors, treatment overlap, and latest research to help patients and clinicians manage both conditions effectively.
read more