
Quercetin Medication Interaction Checker
Check Your Medication Risk
Enter your prescription medications to see if quercetin supplements could interact dangerously with your treatment.
Interaction Results
Why this interaction happens:
What you should do:
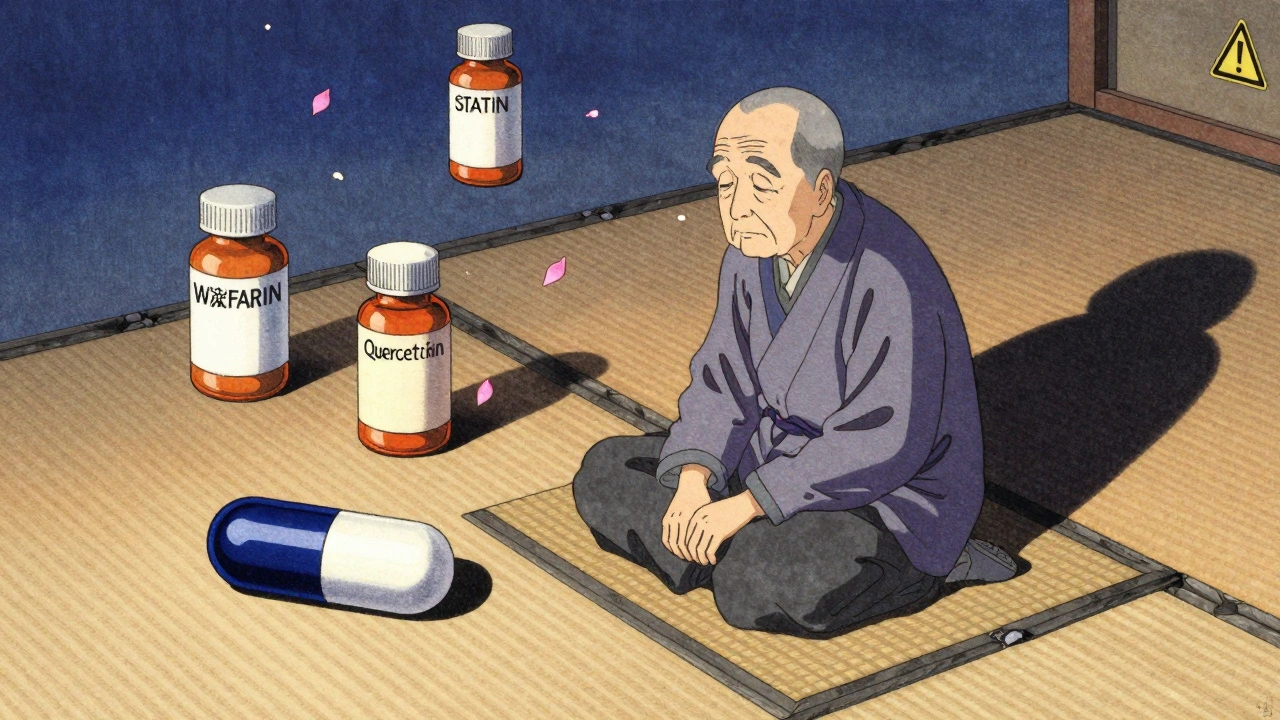
Many people take quercetin supplements hoping to reduce inflammation, boost immunity, or fight allergies. It’s natural, found in apples, onions, and berries, and marketed as a safe, everyday health aid. But here’s the part no label tells you: quercetin can change how your body processes prescription drugs-sometimes dangerously.
If you’re on blood thinners, blood pressure meds, antidepressants, or cancer drugs, taking quercetin could mean your medication builds up in your system. That’s not a myth. It’s science. And it’s happening right now to people who think they’re just taking a harmless supplement.
How Quercetin Slows Down Your Body’s Drug Cleanup
Your liver has a team of enzymes-called cytochrome P450-that break down most medications so your body can get rid of them. Quercetin doesn’t just pass through. It jams the system.
Research shows quercetin strongly blocks CYP2D6, moderately blocks CYP3A4, and also hits CYP2C19. These are the same enzymes that handle over 50% of all prescription drugs. When quercetin gets in the way, drugs like antidepressants, statins, and blood thinners don’t get broken down as fast. That means higher levels stay in your blood longer.
Think of it like traffic. Normally, your body clears drugs off the highway at a steady pace. Quercetin slams on the brakes. Cars pile up. In some cases, drug levels can jump by 30% to 300%. That’s not a small bump. That’s a risk for overdose.
Which Medications Are Most at Risk?
Not all drugs are affected the same. Some are far more vulnerable. Here’s what you need to watch out for:
- Warfarin (Coumadin) - Quercetin can raise INR levels by 0.8 to 1.5 points. That’s enough to cause dangerous bleeding.
- Cyclosporine - Used after organ transplants. Quercetin may raise its levels by 30-50%, increasing kidney damage risk.
- Abemaciclib and other cancer drugs - Used for breast cancer. Quercetin can increase drug exposure by 25-35%, worsening side effects like diarrhea and low blood counts.
- Acenocoumarol - Another blood thinner. Interaction can raise levels by 30-45%.
- Apixaban and Rivaroxaban (DOACs) - Even though they’re newer, quercetin blocks transporters that clear them, raising levels by 20-35%.
- Statins (like atorvastatin) - Risk of muscle damage increases when metabolism slows.
- Antidepressants (SSRIs, TCAs) - Especially those processed by CYP2D6, like fluoxetine or amitriptyline. Higher levels mean more dizziness, heart rhythm issues, or serotonin syndrome.
These aren’t rare cases. In a 2021 study at UCSF, 12 patients on cyclosporine who started quercetin supplements had spikes in blood levels within 72 hours. One needed hospitalization.
Why Food Doesn’t Do This-But Supplements Do
You eat onions and apples every day. You don’t have a drug interaction. Why?
Because the quercetin in food is bound to sugar molecules (glycosides like rutin). Your body absorbs it slowly and in tiny amounts. A cup of onions gives you about 20 mg. Even a large apple? Maybe 10 mg.
Supplements? They pack 500 mg, 1,000 mg, even 2,000 mg per capsule. That’s 50 to 100 times more than you’d get from food. And it’s absorbed fast-directly into your bloodstream.
Plus, many supplements use pure quercetin aglycone, the form that’s most active at blocking enzymes. That’s the same form used in lab studies showing 70-85% inhibition of CYP2D6. Food doesn’t give you that.

Who’s Most at Risk?
It’s not just about what you take. It’s about who you are.
- People over 65 - Your liver and kidneys slow down. Quercetin stays in your body longer. Studies show 25-40% slower clearance.
- People on multiple meds - If you’re taking five or more drugs, you’re more likely to be on one that quercetin interferes with.
- People with liver disease - Your enzyme system is already compromised. Adding quercetin pushes it further.
- People with cancer or transplants - These drugs have razor-thin safety margins. A small rise in level can be life-threatening.
And here’s the scary part: most people don’t tell their doctors they’re taking supplements. A 2021 survey found that 71% of quercetin users never mentioned it to their pharmacist or physician.
What the Experts Say
The European Food Safety Authority (EFSA) warned in 2018: supplements over 1,000 mg/day could cause dangerous interactions.
The FDA labeled quercetin a “dietary supplement of concern” in 2020. They now require drug makers to test for quercetin interactions during approval.
Pharmacists at UCSF and the American Society of Health-System Pharmacists (ASHP) say this: avoid quercetin supplements entirely if you’re on blood thinners, immunosuppressants, or chemotherapy drugs.
Dr. Basheer Kerem, a pharmacology expert at Hebrew University, says intestinal enzyme inhibition from quercetin may be even more important than liver effects. That’s because the first pass of the drug happens right there-before it even enters your bloodstream.
What Should You Do?
If you’re taking any prescription medication and you’re considering quercetin-or already taking it-here’s what to do:
- Stop taking quercetin supplements if you’re on any of the high-risk drugs listed above.
- Don’t assume it’s safe because it’s “natural.” Natural doesn’t mean harmless. Garlic, St. John’s wort, and grapefruit are natural too-and they’re known to cause serious interactions.
- Talk to your pharmacist. They have access to interaction databases your doctor might not check daily. Ask: “Does this supplement interfere with any of my meds?”
- If you must take it (e.g., under medical supervision), keep the dose under 250 mg/day and take it at least 6 hours apart from your medication. This reduces interaction risk by about half.
- Watch for signs of overdose: unusual bruising, dizziness, nausea, irregular heartbeat, extreme fatigue. If you feel off after starting quercetin, stop it and call your doctor.
There’s no reason to risk your health for a supplement that hasn’t proven to be life-saving in any large-scale human trial. The benefits are mostly theoretical. The risks? Very real.
The Bigger Picture
The global quercetin supplement market hit $387 million in 2022. Over 18 million Americans take it. And 42% of them take more than 500 mg a day. That’s over 7 million people at potential risk.
Yet, the FDA has only documented 147 cases of suspected interactions since 2015. Experts believe less than 5% of cases are reported. That means tens of thousands could be affected without anyone knowing.
Regulators are catching up. The FDA is pushing for new labeling rules in 2024 that will require supplement makers to warn about drug interactions. But until then, the burden is on you.
Don’t let marketing fool you. Quercetin isn’t a magic bullet. It’s a potent biochemical actor-and it doesn’t play nice with most medications.
Can I take quercetin if I’m on blood pressure meds?
It depends. Quercetin can interact with some blood pressure medications, especially those metabolized by CYP3A4 or CYP2D6, like amlodipine, metoprolol, or diltiazem. It may raise drug levels and cause low blood pressure, dizziness, or slow heart rate. If you’re on these drugs, avoid quercetin supplements. Talk to your pharmacist before starting.
Is quercetin safe with antidepressants?
No, not reliably. Many antidepressants-like sertraline, fluoxetine, amitriptyline, and venlafaxine-are broken down by CYP2D6, which quercetin strongly blocks. This can lead to toxic buildup, causing serotonin syndrome, heart rhythm problems, or extreme drowsiness. Avoid combining them.
Does quercetin affect blood thinners like Eliquis or Xarelto?
Yes. While quercetin doesn’t directly affect the clotting mechanism, it inhibits transporters (OATP1B1, BCRP) that clear drugs like apixaban and rivaroxaban. This can raise their levels by 20-35%, increasing bleeding risk. The ASHP advises avoiding quercetin entirely if you’re on these drugs.
How long does quercetin stay in the body?
Quercetin and its metabolites can linger for 12-24 hours after a high-dose supplement. For older adults or those with liver issues, it may stay longer. If you’re switching from quercetin to a medication, wait at least 24-48 hours before starting the drug to reduce interaction risk.
Can I get enough quercetin from food without risk?
Yes. Eating onions, apples, capers, berries, and broccoli gives you 10-50 mg per day-far below the 500 mg threshold where interactions begin. Food-based quercetin is bound in forms your body absorbs slowly and safely. No interaction risk from diet alone.
Are there any supplements that are safer than quercetin?
If you want anti-inflammatory support, consider curcumin (from turmeric) or omega-3s. Both have strong evidence for reducing inflammation and much lower interaction risk. Curcumin has minimal effect on CYP enzymes, and omega-3s don’t interfere with drug metabolism at all. Always check with your pharmacist before switching.
Final Takeaway
Quercetin supplements aren’t harmless. They’re biochemical tools that interfere with how your body handles drugs. For most people, the risks far outweigh any unproven benefits. If you’re on medication, skip the supplement. Eat your onions. Stay safe.
Okay but have you ever just... eaten an onion? Like, raw? It’s literally the most aggressive food on earth. If your body can handle that, why is a pill suddenly the devil? 🤔
Look, I get the fear-mongering, but let’s be real-this isn’t some new discovery. Pharmacologists have known about flavonoid-enzyme interactions since the 90s. The real issue is that supplement companies don’t have to prove safety before selling, unlike real drugs. So yeah, quercetin blocks CYP2D6? So does grapefruit juice, and we don’t ban oranges. The problem isn’t the supplement-it’s the lack of regulation. If you’re on warfarin and take a 500mg capsule daily without telling your doctor, that’s on you. But blaming quercetin? That’s like blaming a hammer because someone used it to break a window. The tool’s fine. The user’s the problem.
They don’t want you to know this-but the FDA’s silence on this isn’t oversight. It’s corruption. Big Pharma owns the supplement industry. They let quercetin slide because they know people will stop buying expensive statins if they realize onions work better. The 147 reported cases? That’s the tip of the iceberg. The real numbers are buried in death certificates labeled ‘cardiac arrest’ or ‘undiagnosed liver failure.’ You think they want the public to know that a $10 bottle of capsules could be killing people faster than opioids? No. They’d rather you keep scrolling.
Actually, the data is flawed. The UCSF study cited? It had n=12. One hospitalization. That’s not a trend-that’s an outlier. And the 300% increase claim? That’s from in vitro studies using 100µM concentrations-equivalent to swallowing 12 capsules at once. Real humans don’t do that. Also, CYP2D6 polymorphism means 7% of the population are poor metabolizers anyway-quercetin doesn’t change their risk profile. The real danger? Fear-mongering that makes people abandon proven therapies. Don’t panic. Educate.
India has been using turmeric for 5,000 years-and no one dies from it!! But you Americans? You take one pill and your liver goes on strike!! This is why Western medicine is broken!! You turn EVERYTHING into a crisis!! Quercetin? It’s just a plant compound!! You eat berries, you eat onions, you eat garlic-and you live!! But if you take a capsule? Suddenly it’s a bio-weapon!! This is capitalism!! They sell you fear so you buy more drugs!!
Honestly, I think this whole thing’s overblown. I’ve been taking 500mg of quercetin for two years with my blood pressure med, and I’m fine. I even got my levels checked. No spike. Maybe it’s just not a problem for everyone? Like, not all drugs are affected the same way, and not all bodies process things the same. Maybe the real message is: know your own body. Talk to your pharmacist. Don’t assume the worst.
Let’s cut through the noise: quercetin is a potent, non-selective enzyme inhibitor. The science is unequivocal. CYP2D6 inhibition is well-documented at doses above 250mg. The 2021 UCSF case series? That’s not an outlier-it’s a preview. And the fact that 71% of users don’t disclose this? That’s not negligence-it’s negligence on an epidemic scale. You don’t need a PhD to understand that blocking the liver’s detox pathway while on anticoagulants is like turning off the brakes on a speeding train. This isn’t ‘natural vs synthetic.’ It’s biochemistry. And biochemistry doesn’t care about your wellness blog.
So… what you’re saying is… I shouldn’t take the quercetin I bought because it says ‘boosts immunity’ on the label? But the label also says ‘not evaluated by the FDA.’ So… is this just a giant scam? I’m confused now.
Eat onions. Skip the pills.