Blood clots in stents are a serious concern for patients with peripheral artery disease. This condition, affecting the arteries that supply blood to the limbs, may require an intervention such as the placement of a stent. These tiny tubes help keep arteries open, improving blood flow and aiding in the prevention of further complications.
However, sometimes blood clots can form within these stents. It's a complication that can lead to reduced effectiveness and additional health risks. Understanding why this happens and how it can be prevented is crucial for patients and healthcare providers alike.
- Introduction to Peripheral Artery Disease
- How Stents Work and Their Importance
- Causes of Blood Clots in Stents
- Recognizing Symptoms and Risks
- Prevention and Treatment Options
Introduction to Peripheral Artery Disease
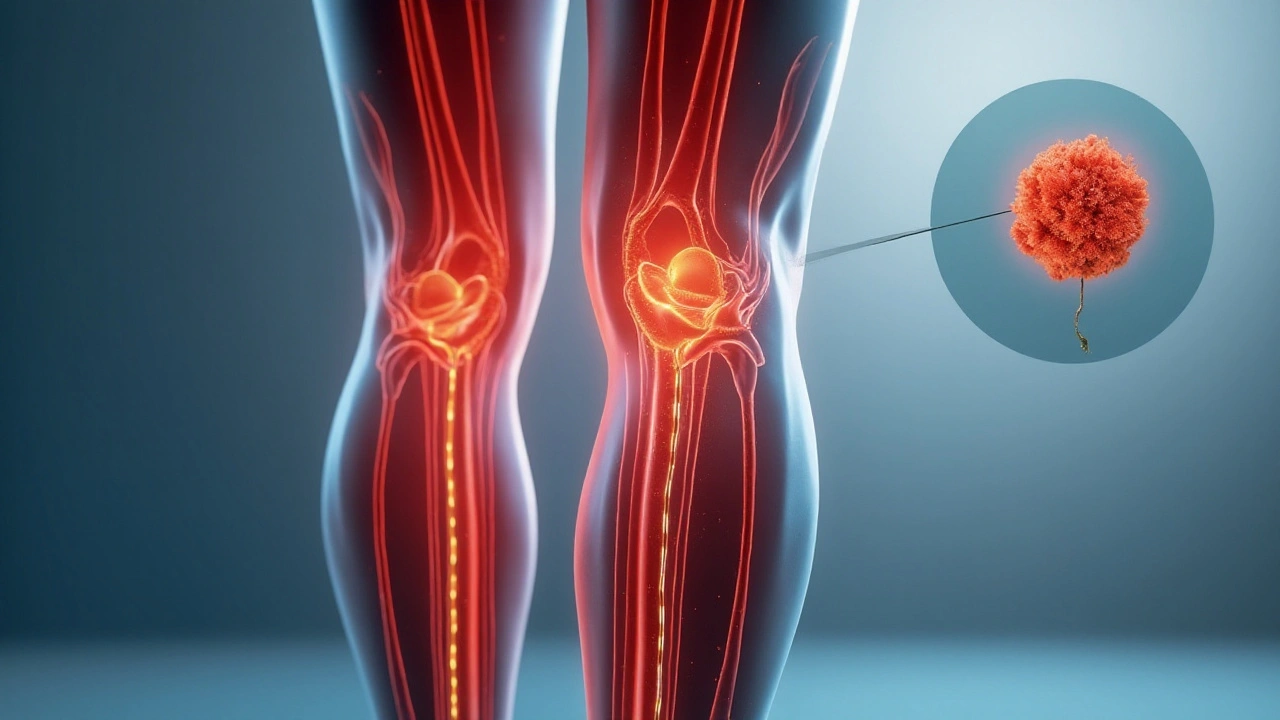
Peripheral artery disease, commonly referred to as PAD, is a condition that sneaks up on many people due to its gradual development and often subtle symptoms. At its core, PAD is a disorder where arteries outside of the heart, typically those that supply blood to the limbs, become narrowed or blocked by fatty deposits known as plaques. This narrowed condition is called atherosclerosis. Although it can develop in any artery, the legs are most commonly affected. It's a bit like traffic congestion at rush hour, but happening inside your body. When blood has trouble moving through these important passageways, the muscles and tissues connected to them suffer from a shortage of oxygen-rich blood.
As the disease progresses, individuals might start to experience leg pain when walking, which can be quite debilitating. This is medically termed claudication, resembling the
How Stents Work and Their Importance
Stents have revolutionized the way we manage cardiovascular diseases, especially conditions like peripheral artery disease. Essentially, a stent is a small mesh tube that's inserted into an artery. Once in place, it acts as a scaffolding to help keep the artery open and support the blood flow. The placement of a stent is generally done through a minimally invasive procedure, often via a catheter. This is designed to be fast and with a shorter recovery time compared to more invasive surgical options. Once inserted, the stent expands to fit the inner wall of the artery, instantly improving the circulation of blood, which is vital in restoring the function of organs and muscles that depend on that blood supply.
Stents come in different types—bare-metal, drug-eluting, and bioresorbable. Each has its own set of indications and benefits. Drug-eluting stents, for example, are coated with medication that is slowly released to prevent the artery from becoming reblocked, a condition known as restenosis. This medication is crucial in reducing the risk of scar tissue forming around the stent which could narrow the artery again. The ability of these stents to deliver drugs directly to the site makes them a highly effective tool against repeat blockages.
The importance of stents cannot be overstated. They have drastically reduced the need for open surgeries, which carry a much higher risk and longer recovery period. According to the American Heart Association, the development of stent technology has significantly increased survival rates in patients with severe heart and arterial conditions.
"In many cases, stent placement can prevent the need for coronary artery bypass surgery, a much more invasive procedure," explains Dr. Robert Siegel, a noted cardiologist.
Apart from keeping arteries open, the role of stents extends to reducing the symptoms associated with blockages. Patients often find instant relief from symptoms like chronic pain and fatigue in their limbs. This improvement in quality of life is one of the reasons why stents are so widely used. The direct consequence of better blood flow is increased mobility and reduced risk of complications like limb amputation. However, they are not permanent fixes—they require the patient to follow strict medical guidance to avoid complications like the development of blood clots in stents.
Interestingly, the adoption and usage statistics of stents have shown an upward trend. A report by the Centers for Disease Control and Prevention noted a 15% increase in stent insertions over the last decade. These figures point to the effectiveness and trust healthcare professionals place in this technology. It's worth noting, though, that stent placement should come with a comprehensive aftercare plan to ensure the long-term success of the procedure.

Causes of Blood Clots in Stents
The occurrence of blood clots in stents is a complex issue and involves various factors that can interfere with the natural healing process intended by the placement of these devices. Several mechanisms lead to clot formation, a situation known in medical terms as stent thrombosis. Understanding these causes can help in mitigating the risks and ensuring stents perform their critical function in managing peripheral artery disease.
One primary cause is the body's natural response to a foreign object. When a stent is placed inside an artery, the body sometimes perceives it as an intruder, triggering an immune response. This defense mechanism, while meant to protect us, can actually lead to blood clot formation. As the cells congregate at the site thinking it's an injury needing repair, they might end up creating a blockage instead. Additionally, the formation of blood clots can be significantly influenced by certain medical conditions such as diabetes or high cholesterol, which are prevalent among individuals with peripheral artery disease.
Another critical contributing factor is inadequate endothelialization. This is the process where the artery's lining grows over the stent, incorporating it into the vessel wall. If this process is incomplete or slow, exposed metal surfaces can attract particles in the blood, such as platelets, which aggregate to form clots. It's important to note that the type of stent used, whether bare-metal or drug-eluting, can also alter how efficiently this process is completed. Drug-eluting stents, while effective at preventing re-narrowing of the artery, may delay endothelial coverage, thus increasing the clotting risk.
Regular medication adherence is crucial in preventing stent thrombosis. Antiplatelet therapy, often prescribed post-stent placement, helps in reducing this risk by preventing platelet aggregation. Unfortunately, not all patients adhere strictly to this regimen. A startling statistic emerges from a recent study, showing that non-adherence to prescribed antiplatelet therapy can increase the risk of stent thrombosis by over 50%. This highlights the importance of educating patients on the significance of maintaining their medication schedule diligently.
A study published in the Journal of the American College of Cardiology states, "The incidence of stent thrombosis can be drastically reduced with improved adherence to dual antiplatelet therapy.”
There are also lifestyle choices that influence clot formation in stents. Inactivity, smoking, and a poor diet can slow circulation, leading to an increased risk of clot development. This emphasizes the importance of holistic care and lifestyle changes, alongside medical treatment, to lower the incidence of clotting complications. Ensuring patients are supported in making these changes is a crucial aspect of their care.
Recognizing Symptoms and Risks
When dealing with peripheral artery disease and blood clots in stents, recognizing symptoms early can be life-changing. Symptoms can often be subtle at first, making it important to pay close attention to how you’re feeling. Many patients report feeling unusual pain or discomfort in the affected limb, which can be similar to the sensations felt before stent placement but may be more intense or persistent. These symptoms are commonly a result of blood flow being restricted once again due to clot formation. It’s crucial not to dismiss these signs as merely part of the healing process.
Dizziness or a sudden tightness in the chest can also be warning signals. Though these might seem unrelated, they can indicate a more systemic response to developing complications in your circulatory system. Health experts often warn that such symptoms, when coupled with shortness of breath or increased heart rate, may not just signal an issue with your peripheral arteries but could be a precursor to larger complications such as cardiovascular incidents. Monitoring changes in your physical condition and reporting them to a healthcare provider can significantly increase the chances of early intervention.
One should also be alert to changes in skin color or temperature in the limb where the stent is placed. Sometimes, parts of the leg or arm may become cooler to the touch, or bear a pale or bluish tint, indicating compromised blood circulation. Swelling is another indicator not to ignore. Identifying these signals promptly can help in averting more severe outcomes. The presence of a clot can escalate if your body’s signals are overlooked. A number of practitioners suggest maintaining a daily check-in diary to track any changes or discomfort as a mechanism to better manage the risks involved.
Dr. Sheila Williams from the National Heart Institute advises, "Patients must stay connected with their bodies post-stent placement. Being acutely aware of your baseline and then identifying any deviations from it can be the simplest yet most effective way to manage potential complications."
Being aware of the risks is as critical as recognizing the symptoms. Those with lifestyle factors such as smoking, high cholesterol, and diabetes should consider themselves at heightened risk. These elements can exacerbate the likelihood of blood clots forming, impacting the stent's efficacy. Maintaining a healthy diet, regular physical activity, and adherence to medication can significantly curtail these risks. In some cases, doctors indeed recommend medications specifically aimed at reducing clot formation within stents. Such preventive measures often form part of a broader ongoing management plan that encompasses all aspects of the patient's lifestyle and medical background.

Prevention and Treatment Options
When it comes to preventing blood clots in stents for patients with peripheral artery disease, the most effective strategy often begins with a healthy lifestyle. Emphasizing a diet that is low in cholesterol and saturated fats can significantly reduce the risk of clot formation. Regular exercise, tailored to individual capabilities, also plays a key role in maintaining optimal blood flow and vascular health. Physicians often recommend a combination of these practices alongside medications aimed at thinning the blood and reducing inflammation within the arteries.
A critical facet of managing this condition involves regular follow-up appointments with healthcare providers. These check-ups can help monitor the function of the stents and the health of the arteries, ensuring that any potential issues are addressed promptly. It's also essential for patients to report any unusual symptoms, such as swelling, pain, or discoloration in the limbs, as these may signal a blockage. This proactive approach can make a big difference in long-term outcomes, allowing for any necessary interventions to be implemented swiftly.
In terms of treatment, anticoagulant and antiplatelet medications are frequently prescribed. These drugs, such as aspirin and clopidogrel, work by preventing platelets from clumping together. This reduces the likelihood of a blood clot forming within the stent. For some patients, more advanced therapies like dual antiplatelet therapy (DAPT) may be recommended. This approach combines the effects of two medications to maximize protection against clot formation.
Sometimes, more interventional management might be required. This can include procedures like angioplasty, where a balloon is used to widen the narrowed artery, or even more complex surgeries in severe cases. These interventions aim to restore adequate blood flow and prevent further complications, serving as crucial tools in the management of peripheral artery disease. It’s important to note that each treatment plan is individualized, taking into account the patient’s health, the severity of the disease, and their personal preferences.
A study in the Journal of the American College of Cardiology found that "patients who rigorously adhere to their medication and lifestyle recommendations show significantly better outcomes." This underscores the importance of a collaborative effort between patients and their healthcare teams, promoting open communication and active participation in the treatment process. By staying informed and engaged, patients can play a pivotal role in managing their health, potentially avoiding the adverse effects associated with blood clots in stents.
In addition to these treatments, some patients may benefit from new technologies and techniques being developed in the field of vascular care. Researchers are continually exploring innovative solutions, including bioresorbable stents and drug-coated options, which aim to improve long-term outcomes and reduce complications. Keeping abreast of these advancements could offer additional pathways for ensuring healthier lives for those managing this challenging condition.
Stent thrombosis serves as a stark reminder that the job isn’t done once the metal is in place. You need to lock down antiplatelet therapy, quit smoking, and keep arteries moving with regular exercise. Ignoring any of those pillars invites the clot to form faster than you think. Think of it as a team sport – every player must show up for the win.
America leads in vascular tech but we still let patients skip pills and pay the price. The science is crystal clear – stick to dual antiplatelet or face inevitable blockage.
When a foreign scaffold intrudes upon the arterial wall, the body reacts with the ferocity of a medieval siege. Endothelial cells, the peaceful citizens of the vessel interior, are forced to retreat behind a metallic barricade. Platelets, ever‑vigilant soldiers, swarm the exposed steel like a legion preparing for battle. If the protective endothelial curtain fails to drape over the stent in a timely fashion, the clotting cascade erupts unchecked. Diabetes and hyperlipidemia act as treacherous allies, accelerating the formation of a toxic fibrin net. Even the most sophisticated drug‑eluting stent can become a double‑edged sword, releasing medication that delays healing while staving off restenosis. Patients who abandon their antiplatelet regimen are essentially cutting the rope that holds the storm at bay. Studies show that non‑adherence spikes the risk of thrombosis by more than fifty percent, a figure that should shock even the most stoic clinician. Yet, lifestyle choices-sedentary habits, nicotine, and a diet rich in saturated fats-still linger as silent architects of clot. Physicians who neglect to emphasize comprehensive after‑care are complicit in the tragedy that follows. Imaging follow‑up, such as duplex ultrasound, can catch an incipient thrombus before it declares war on the limb. When caught early, catheter‑directed thrombolysis or a repeat angioplasty can restore flow without resorting to amputation. Conversely, delayed intervention often culminates in limb loss, a price far exceeding the inconvenience of daily medication. The moral is simple: a stent is not a set‑and‑forget device; it is a living partnership. Patients must honor the regimen, physicians must monitor diligently, and researchers must innovate smarter scaffolds. Only through this triad can we hope to silence the clamor of clot formation inside our arteries.
It's easy to feel overwhelmed when the aftermath of a stent placement demands constant vigilance. The emotional toll of daily medication can be just as taxing as the physical risk. Rest assured, adhering to the regimen drastically reduces the chance of re‑occlusion, and support groups often provide the encouragement needed to stay the course.
While the patriotic spirit fuels our pride in medical innovation, the reality on the ground is that compliance falters when patients are left in the dark. A comprehensive discharge plan that details dosage schedules, potential side effects, and the importance of lifestyle modification can bridge that gap. Moreover, integrating community health workers to conduct follow‑up visits has shown measurable improvements in adherence rates. In regions where such outreach is lacking, the incidence of stent thrombosis climbs steeply, reinforcing the notion that technology alone cannot save lives. Therefore, policymakers must allocate resources not just for the procedure but also for the post‑procedural ecosystem that sustains patient health.
One could argue that focusing solely on clots distracts from the broader issue of systemic atherosclerosis. Even with a perfectly endothelialized stent, an untreated plaque burden will eventually jeopardize vessel integrity. A holistic approach targeting lipid management and inflammation may yield better long‑term outcomes than anticoagulation alone.
Skipping antiplatelet pills guarantees a clot.
From a hemodynamic perspective, shear stress alterations post‑stent placement predispose to platelet activation, especially in regions of turbulent flow. Incorporating computational fluid dynamics into pre‑procedure planning could identify zones at heightened thrombotic risk. Tailoring drug‑elution profiles to those micro‑environments may further mitigate the pro‑coagulant cascade.
Life mirrors the stent: we often think a single reinforcement will suffice, yet neglect the surrounding currents that constantly threaten collapse. By acknowledging the interdependence of medication, movement, and mindset, we cultivate a more resilient vascular ecosystem. In this way, the patient becomes an active participant in their own circulatory narrative.
I've seen countless patients regain confidence once they commit to their antiplatelet schedule 😊. Small daily habits build a fortress against the lurking threat of thrombosis.
Behold, the silent assassin that is stent thrombosis, lurking beneath the veneer of modern medicine! Only through unwavering discipline and vigilance may we hope to vanquish this hidden foe. Let us pledge to honor the sanctity of our vessels with steadfast adherence.
Evidence‑based protocols dictate a minimum of 12 months of dual antiplatelet therapy for drug‑eluting stents in peripheral arteries, unless contraindicated. Deviations from this guideline should be justified by robust risk‑benefit analyses, incorporating platelet function testing where appropriate.
While the mainstream narrative praises antiplatelet drugs, few acknowledge the covert influence of pharmaceutical lobbying on these recommendations. A discerning patient should scrutinize the literature, questioning the true motives behind prolonged medication mandates. Ignorance, after all, is the most profitable commodity in the healthcare market.