
Every year, thousands of children end up in emergency rooms because their parents gave them too much of a medicine - not because they meant to, but because they didn’t know they were giving the same thing twice. It sounds simple: read the label, give the right dose. But when you’re tired, stressed, or juggling multiple kids, it’s easy to mix up what’s in each bottle. Active ingredients are the real culprits behind most double dosing accidents, and most parents don’t even know what to look for.
Why Double Dosing Happens (and Why It’s Dangerous)
Double dosing doesn’t always mean giving two full doses. Sometimes it’s as simple as giving a fever reducer and a cold medicine that both contain acetaminophen. Or giving a sleep aid and a cough syrup that both have diphenhydramine. These aren’t rare mistakes - a 2016 study in Pediatrics found that 21% of parents have accidentally given their child too much medicine at least once. And the numbers keep climbing. Children, especially those under 5, are more vulnerable because their bodies process medicine differently. A dose that’s safe for an adult might be dangerous for a 20-pound toddler. For example, acetaminophen (also called paracetamol or APAP) has a very narrow safety window. Giving more than 150 mg per kilogram of body weight can cause serious liver damage. And here’s the scary part: many common cold and flu products contain acetaminophen. NyQuil, Theraflu, Vicks DayQuil, and even some children’s allergy syrups all have it. Parents think they’re giving something different - but the active ingredient is the same. Ibuprofen is another big one. It’s in Advil, Motrin, and many combination cold formulas. If you give Motrin for fever and then give a nighttime cold medicine later that night, you might be doubling up without realizing it. And when you mix acetaminophen and ibuprofen to alternate doses - which some parents think is safer - you actually increase the risk of error by 47%, according to the American Academy of Family Physicians.The Most Common Culprits: What to Look For
There are only a few active ingredients that cause the majority of double dosing incidents. If you know these, you can avoid 90% of the risks.- Acetaminophen (also listed as APAP, paracetamol, or N-acetyl-p-aminophenol) - found in Tylenol, Excedrin, NyQuil, Theraflu, Vicks, and many children’s cold and flu products.
- Ibuprofen - found in Advil, Motrin, and many multi-symptom cold medicines.
- Diphenhydramine - an antihistamine in Benadryl, Children’s NyQuil, and some nighttime cough syrups. It causes extreme drowsiness and can be dangerous if combined with other sedatives.
- Pseudoephedrine - a decongestant in Sudafed, Claritin-D, and some cold formulas. Can raise heart rate and blood pressure.
- Dextromethorphan - a cough suppressant in Robitussin, Delsym, and many OTC cough syrups. Overdose can cause hallucinations and seizures in kids.
How to Check Active Ingredients - A Simple System
The easiest way to avoid double dosing is to make checking active ingredients a habit. Here’s how:- Read the label before you give anything. Don’t just look at the brand name. Flip the bottle. Look for the section that says “Active Ingredients.” That’s where the real info is.
- Write it down. Keep a small list in your phone or on a sticky note near the medicine cabinet. Note the medicine name, active ingredient, strength (e.g., 160 mg/5 mL), and time given. Update it every time you give a dose.
- Use the measuring tool that comes with the medicine. Household teaspoons vary wildly - some hold as little as 2.5 mL, others as much as 7.5 mL. The FDA says this is why 30% of dosing errors happen. Always use the dropper, syringe, or cup that came with the bottle.
- Assign one person to give medicine. If two caregivers are involved, one person handles all doses. No exceptions. Communication gaps cause 38% of double dosing incidents.
- Ask the pharmacist. When you pick up a new medicine, ask: “Does this have the same active ingredient as [insert medicine name]?” Most pharmacists now offer printed dosing charts with active ingredients highlighted. Use them.

What About Combination Medicines?
The bigger problem today isn’t single medicines - it’s combination products. A single bottle of “Children’s Cold & Flu” might contain acetaminophen, dextromethorphan, and pseudoephedrine. That’s three active ingredients in one dose. If you give that and then also give a separate fever reducer, you’re likely overdosing. The American Academy of Pediatrics says: Don’t use combination cold medicines in children under 6. They don’t work well, and they’re risky. If your child has a runny nose, a cough, and a fever - treat one symptom at a time with a single medicine. Don’t reach for the “everything in one” bottle.Real Stories, Real Consequences
One mother on Reddit shared that her 3-year-old became unresponsive after getting Benadryl for allergies and then a cough syrup with diphenhydramine two hours later. She didn’t know both had the same ingredient. Her child was rushed to the ER and spent the night under observation. Another parent, a nurse, accidentally doubled her 2-year-old’s acetaminophen dose because she gave Tylenol for fever, then gave a nighttime cold syrup without checking the label. She later said: “I thought I was being careful. I didn’t even think to look at the active ingredients.” But there are success stories too. One dad, who works in pharmacy, created a simple chart of all the medicines in his house, listed the active ingredients, and laminated it. He now keeps it on the fridge. Since then, he hasn’t had a single dosing error. His family’s error rate dropped to zero.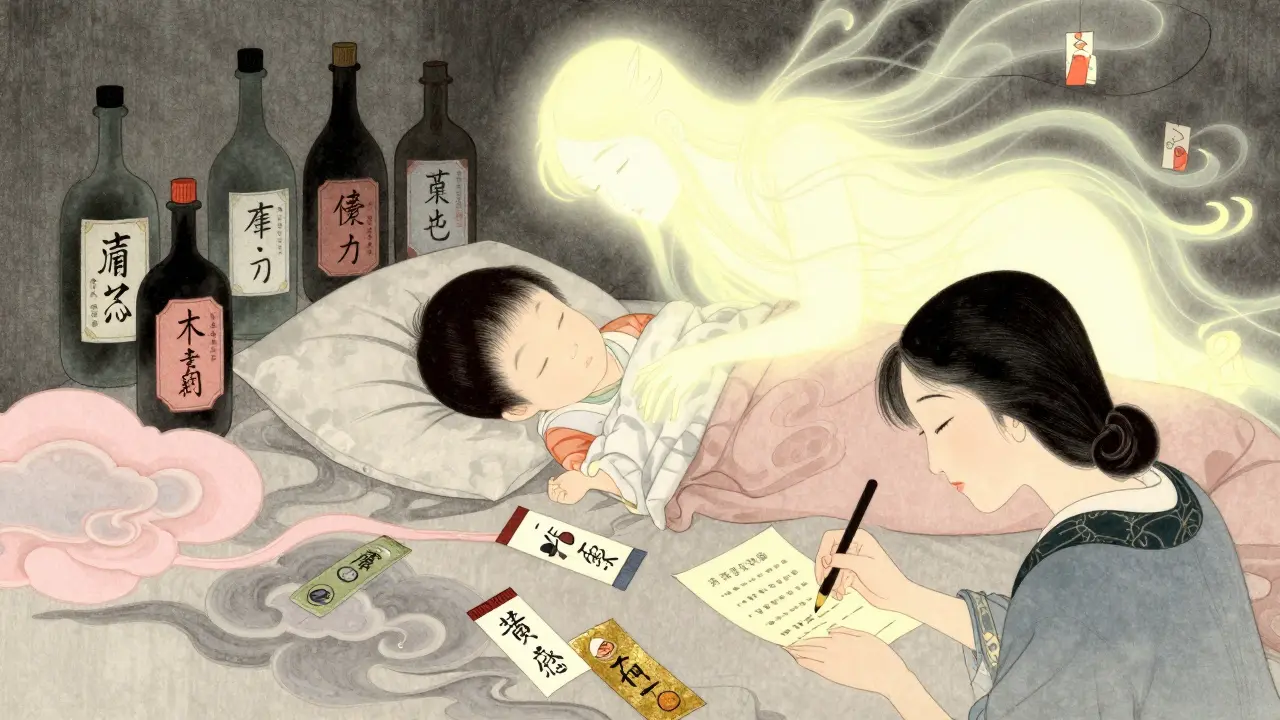
What’s Changing? New Tools and Rules
The FDA is starting to step in. By December 2025, all OTC children’s medicines must list active ingredients in bold, standardized format. No more hiding them in tiny print. And in January 2024, the American Academy of Pediatrics launched the “Know Your Ingredients” campaign - with new icons on packaging to help parents spot acetaminophen, ibuprofen, and diphenhydramine at a glance. Some apps like Medisafe and Round Health now scan barcodes and warn you if you’re about to double up. Amazon Pharmacy’s “MedCheck” feature does the same when you order online. Early data shows these tools have prevented over 12,000 potential overdoses in just six months. But technology alone won’t fix this. The real solution is awareness. You don’t need an app. You don’t need to be a pharmacist. You just need to look at the label - every time.What to Do If You Think You’ve Double Dosed
If you realize you gave your child too much medicine:- Don’t wait for symptoms.
- Call Poison Control immediately: 1-800-222-1222.
- Have the medicine bottle ready - they’ll need the active ingredient and strength.
- Do not induce vomiting unless told to.
Double dosing isn’t about being careless. It’s about not knowing what to look for. Once you learn the five key active ingredients, and make checking them part of your routine, you’ve done more than most parents. You’ve protected your child.
What’s the most common active ingredient that causes double dosing in children?
Acetaminophen (also called paracetamol or APAP) is the most common cause of double dosing in children. It’s found in over 200 different OTC products, including Tylenol, NyQuil, Theraflu, and many children’s cold and flu syrups. Because it’s in so many products, parents often don’t realize they’re giving it twice - especially when using combination medicines.
Can I alternate acetaminophen and ibuprofen to reduce fever?
While some parents alternate acetaminophen and ibuprofen thinking it’s safer, research shows this increases the risk of double dosing by 47%. It’s harder to keep track of timing, and caregivers often misremember which medicine was given last. The American Academy of Pediatrics recommends using one medicine consistently unless directed by a doctor. If you do alternate, write down each dose and time to avoid confusion.
Are children’s liquid medicines always the same strength?
No. Strengths vary widely. For example, children’s acetaminophen can be 160 mg per 5 mL, 80 mg per 1 mL, or even 120 mg per 5 mL. Ibuprofen can be 50 mg per 1.25 mL or 100 mg per 5 mL. Always check the label. Never use an adult dose or a different product’s measuring tool. The only safe way is to use the device that came with the medicine.
Why do some medicines have different names for the same ingredient?
Acetaminophen is listed under 15 different names, including paracetamol, APAP, and N-acetyl-p-aminophenol. This confusion is intentional - manufacturers use different terms to make products seem unique. But they’re the same chemical. If you see any of these names on a label, treat them as the same active ingredient. Always look for the chemical name, not the brand.
Do I need to check active ingredients for prescription medicines too?
Yes. Many prescription medications for children - like ADHD drugs or antibiotics - can interact with OTC medicines. For example, giving a child with ADHD a cold medicine containing pseudoephedrine while on methylphenidate can raise heart rate dangerously. Always tell your pediatrician or pharmacist about every medicine your child takes - even herbal supplements and vitamins.