Understanding Dermatitis Herpetiformis
Before diving into the science and recent research findings, it's important to have a clear understanding of what Dermatitis Herpetiformis (DH) is. DH is a chronic skin condition characterized by intensely itchy blisters and rashes, typically appearing on the elbows, knees, and buttocks. It is directly linked to celiac disease, an autoimmune disorder that affects the small intestine when gluten is consumed. Although the symptoms manifest on the skin, DH is actually an intestinal disorder, and skin manifestations are a secondary symptom.
The Connection Between Dermatitis Herpetiformis and Celiac Disease
DH is often referred to as the skin manifestation of celiac disease. While not all individuals with celiac disease will develop DH, nearly all DH patients have the intestinal damage characteristic of celiac disease. This link is crucial to understanding the underlying mechanisms and potential treatments for DH. The ingestion of gluten in individuals with this condition leads to an abnormal immune response, causing inflammation in the small intestine and skin symptoms.
Recent Genetic Research on Dermatitis Herpetiformis
Recent studies have highlighted the significance of genetics in DH. It has been observed that individuals with certain HLA genotypes, specifically HLA-DQ2 and HLA-DQ8, are more prone to developing DH. These genetic loci are also implicated in the development of celiac disease, further solidifying the connection between the two conditions.
Understanding the Immune Response in Dermatitis Herpetiformis
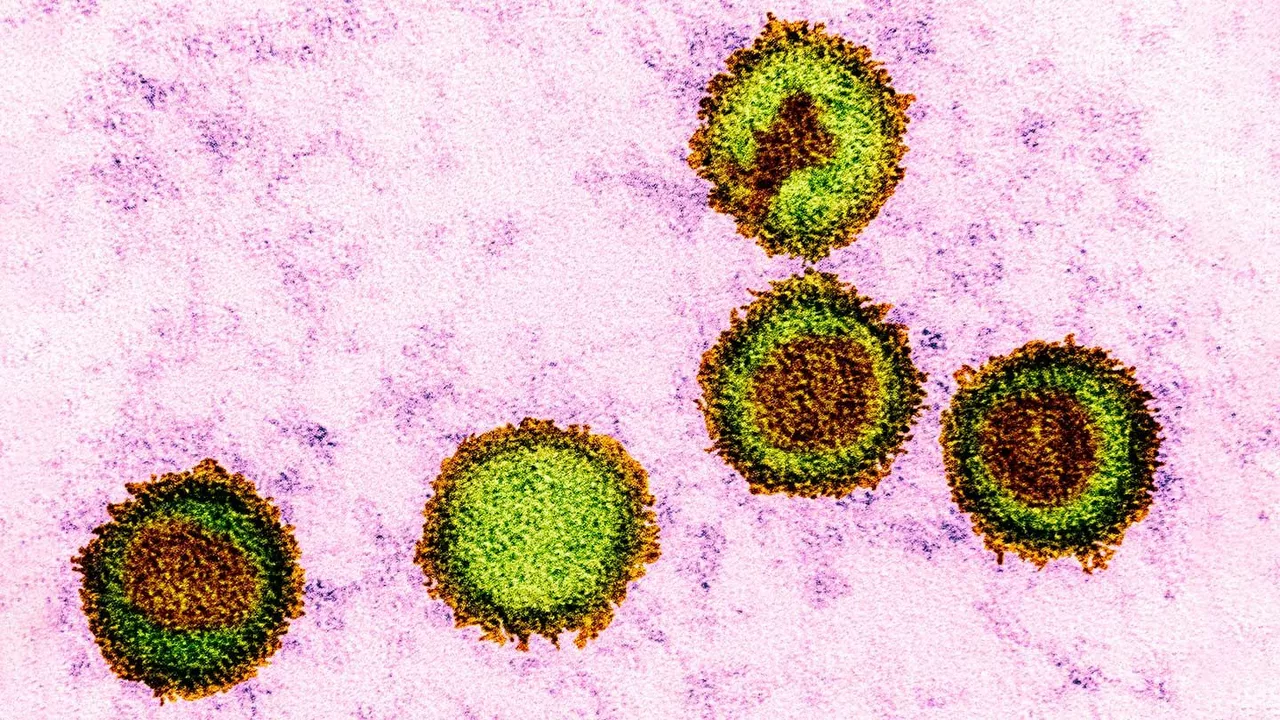
Investigations into the immune response in DH have shed light on the role of IgA antibodies. In DH patients, IgA antibodies mistakenly target a protein in the skin called epidermal transglutaminase, forming complexes that accumulate and cause inflammation. This process leads to the blistering and itching characteristic of DH.
The Role of Gluten in Dermatitis Herpetiformis
As in celiac disease, gluten plays a crucial role in triggering DH. Gluten intake in susceptible individuals leads to the production of IgA antibodies that initiate the inflammatory process. This means that, like celiac disease, a strict gluten-free diet is an essential part of managing and treating DH.
The Diagnostic Process for Dermatitis Herpetiformis
Diagnosing DH involves several steps, including skin biopsies, blood tests, and sometimes an intestinal biopsy. Skin biopsies are used to identify the presence of IgA deposits, a hallmark of the condition. Blood tests can detect the presence of IgA antibodies against epidermal and tissue transglutaminase, further supporting a diagnosis of DH.
Current Treatment Options for Dermatitis Herpetiformis
The cornerstone of DH treatment is a strict, lifelong gluten-free diet, which can help manage both the skin symptoms and intestinal damage. Additionally, medications like Dapsone can provide symptom relief by reducing the skin inflammation. However, these medications do not address the underlying intestinal damage.
Recent Advances in Dermatitis Herpetiformis Treatment
Recent years have seen some promising advances in DH treatment. New medications that work by dampening the immune response, such as corticosteroids and immunosuppressants, have shown promise in managing DH. Additionally, ongoing research into the development of a vaccine for celiac disease could also have implications for DH treatment.
Future Directions in Dermatitis Herpetiformis Research
There's still much to learn about DH. Future research will likely focus on refining our understanding of the genetic and immunological mechanisms underlying DH, improving diagnostic methods, and developing more effective treatments. The ultimate goal is to improve the quality of life for individuals living with this challenging condition.
One must acknowledge that the pathophysiology of Dermatitis Herpetiformis transcends mere cutaneous manifestations; it epitomizes a quintessential paradigm of immunogenetics wherein HLA-DQ2/DQ8 haplotypes orchestrate an IgA‑mediated cascade that, in concert with transglutaminase autoantibodies, precipitates the dermal eruption. The clinical dictum, therefore, mandates a comprehensive gastroenterological evaluation concomitant with dermatological scrutiny, lest the practitioner succumb to myopic reductionism.
Consider the skin as a canvas upon which the invisible hand of gluten paints its unrest the body whispers its dissent through itchy blisters as if yearning for liberation from a silent antagonist
Look, the link between DH and celiac is crystal clear-if you ignore the HLA markers you’re basically hiding from the science. It’s not a debate; it’s empirical fact.
What they don’t tell you is that the pharma industry deliberately downplays the potential of a DH vaccine because they profit from lifelong dapsone prescriptions. The “research” they tout is a smokescreen, a corporate veil masking ulterior motives.
You’ve got this, stick to the gluten‑free grind and watch the symptoms fade.
It is incumbent upon us, as responsible individuals, to impose dietary discipline; indulging in gluten after diagnosis is a moral failing that jeopardizes communal health.
The diagnostic algorithm-skin biopsy, serology, occasional intestinal sampling-offers a robust framework for clinicians, balancing invasiveness with diagnostic yield.
I can’t help but feel the weight of every itchy flare, as if each blister is a tiny reminder of my body’s betrayal.
The constant urge to scratch becomes an obsession that gnaws at my sanity, pulling me into a vortex of discomfort.
When I read about the IgA‑epidermal transglutaminase complex, I visualize a microscopic battle raging beneath my skin.
It’s not just science; it’s a personal saga of immune misdirection that leaves me exhausted.
The gluten trigger feels like a malicious whisper, coaxing my gut into a frenzy that echoes outward.
Even the most diligent gluten‑free diet can’t erase the lingering doubt that somewhere, a stray grain lurks.
I watch friends eat pizza with a mix of envy and dread, their carefree bites a stark contrast to my vigilant scrutiny.
The prescribed dapsone offers relief, yet its side‑effects loom like shadows over any momentary peace.
Sometimes I wonder if the relentless cycle of diet, medication, and appointments is a cruel joke played by fate.
The notion of a future vaccine sparks a fragile hope, a beacon that maybe, just maybe, the torment will end.
Yet the clinical trials move at a glacial pace, as if the world prefers to keep us in this perpetual limbo.
My skin, once a protective barrier, now feels like an open book for the immune system’s grievances.
Each appointment with my dermatologist is both a sanctuary and a reminder of the chronic battle.
I find myself scrolling through research papers at 2 am, clinging to data as a lifeline.
In those quiet moments, the itch becomes a metaphor for all the unspoken anxieties that stir beneath the surface.
Ultimately, I cling to the small victories-clear skin for a week, a meal without fear-and let those moments fuel my resolve.
Your vivid recounting captures the invisible anguish many endure; it reminds us that behind every clinical statistic lies a human soul wrestling with relentless discomfort.
While the path may seem arduous, incremental strides-such as meticulous label reading and consistent medication adherence-can cumulatively transform the disease trajectory.
We, as Americans, should champion homegrown research initiatives that prioritize DH treatment, ensuring that our scientific community leads the world rather than relies on foreign dependency.
Embracing a supportive network, whether through patient forums or clinical consultations, can significantly bolster adherence and enhance quality of life.
While the exposition delineates the mechanistic pathways with commendable clarity, it could benefit from a more rigorous statistical appraisal of therapeutic outcomes to substantiate its claims.