
When you’re breastfeeding, every pill, injection, or patch you take feels like it could affect your baby. You might wonder: How do medications even get into breast milk? And if they do, is it dangerous? The truth is, most medications pass into breast milk in tiny, harmless amounts-but not all. Understanding how this works can help you make confident choices without stopping breastfeeding unnecessarily.
How Medications Get Into Breast Milk
Medications don’t magically appear in breast milk. They travel from your bloodstream, through the walls of blood vessels near your milk-producing cells, and into the milk itself. The main way this happens is through passive diffusion. About 75% of drugs move this way-just flowing from where there’s more (your blood) to where there’s less (your milk), following a natural concentration gradient.
But not all drugs follow the same path. Some use special transporters in your breast tissue, like a delivery system built into your body. Drugs like nitrofurantoin and acyclovir use these channels. Others are too big to fit through-anything over 800 daltons, like heparin, barely gets in at all. That’s why blood thinners like heparin are considered safe during breastfeeding: they’re too large to cross.
Another big factor is how easily a drug dissolves in fat. Medications that love fat (lipophilic), like diazepam, slip into milk more easily than water-soluble ones like gentamicin. That’s why diazepam can show up in breast milk at levels 1.5 to 2 times higher than in your blood, while gentamicin stays below 10%.
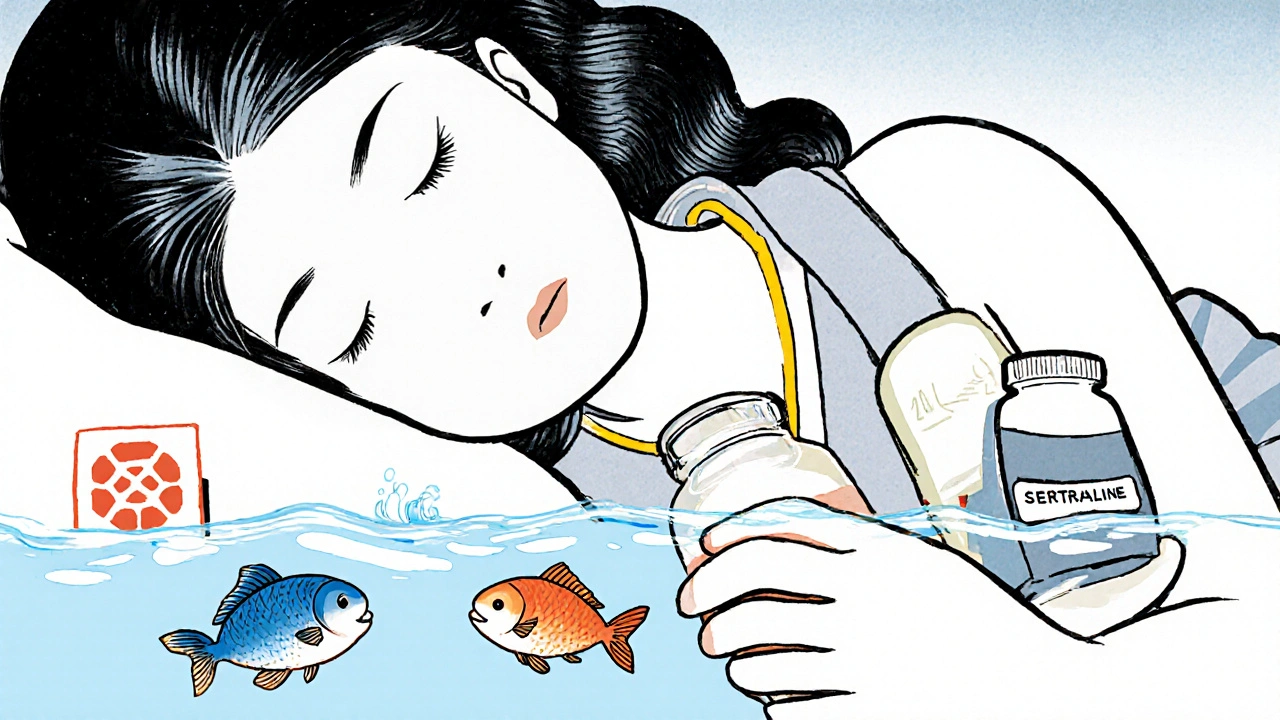
Protein binding matters too. If a drug sticks tightly to proteins in your blood-like warfarin, which binds to over 99% of proteins-it doesn’t float freely to enter milk. That’s why warfarin transfers less than 0.1% of your dose. But sertraline, even though it’s 98.5% bound, still makes it into milk because that tiny unbound portion is enough to pass through.
There’s also something called ion trapping. If a drug is a weak base (like amitriptyline), and your milk is slightly more acidic than your blood, the drug gets trapped in the milk and builds up. That’s why some antidepressants show up in milk at 2 to 5 times the concentration in your blood.
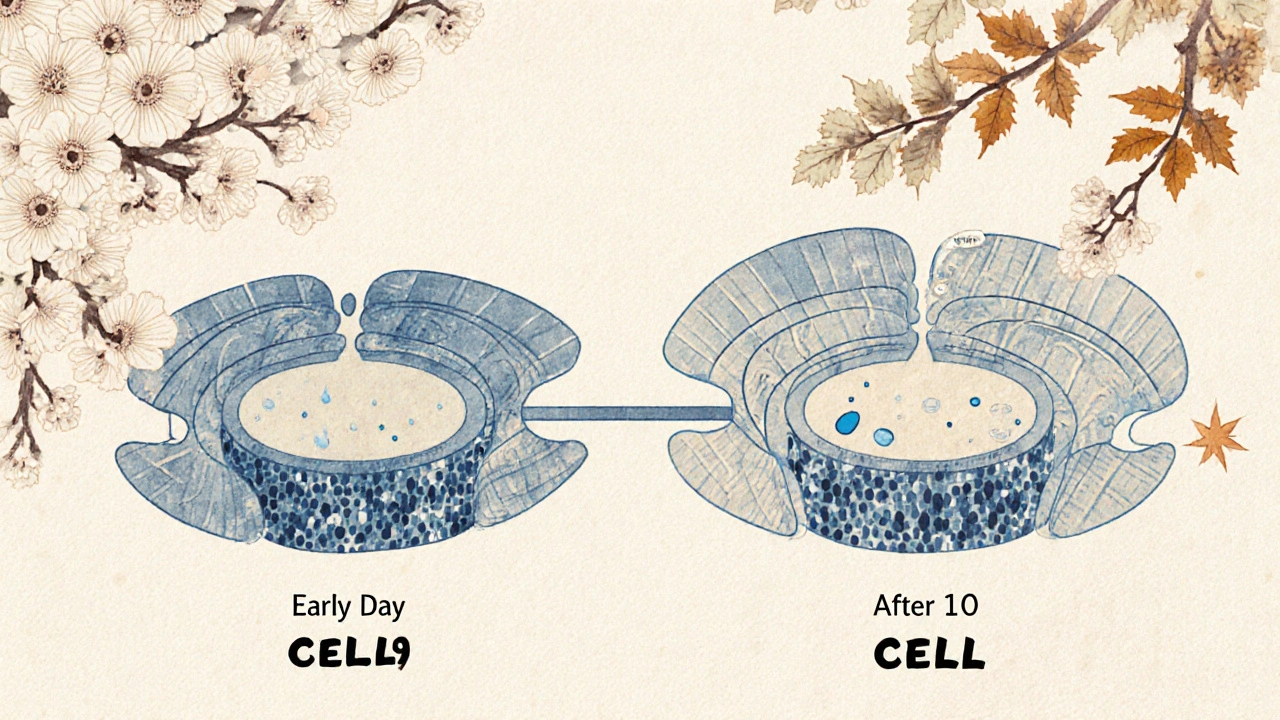
And here’s something most people don’t know: right after birth, your breast tissue is still developing. Between days 4 and 10, tiny gaps between milk-producing cells are wider-up to 20 nanometers. That lets even larger molecules sneak through. After day 10, those gaps close, and transfer drops by 90%. So timing matters. If you start a new medication early postpartum, your baby might get more than if you started it a month later.
How Much Actually Reaches Your Baby?
It’s easy to panic when you hear a drug is in breast milk. But the amount your baby gets is usually tiny. Most medications result in infant exposure under 10% of the mother’s weight-adjusted dose. For many drugs, it’s less than 1%.
Let’s look at real numbers. If you take amoxicillin, your baby gets about 1.5% of your dose. For gentamicin? Just 0.1%. That’s why antibiotics like these are almost always safe. Even SSRIs like sertraline, often feared, result in infant exposure of only 1-2% of your dose. In fact, sertraline is the most commonly prescribed antidepressant for breastfeeding mothers because of its low transfer rate.
But some drugs are different. Diazepam, a benzodiazepine, can reach 7.3% of your dose in milk-and because it stays in a baby’s system for 30 to 100 hours (compared to 20-100 in adults), it can build up. That’s why high doses or long-term use need monitoring. Phenobarbital? It can accumulate at 15% per week in newborns. That’s why doctors avoid it unless absolutely necessary.
The CDC says if your baby receives less than 10% of your weight-adjusted dose, the risk is generally low. But it’s not just about quantity-it’s about the baby’s age and health. A newborn’s liver and kidneys are still learning how to process drugs. So even small amounts can affect them more than an older infant.
What Medications Are Safe? What Should You Avoid?
There’s a clear system doctors use to rate medication safety during breastfeeding. The most trusted is the Lactation Risk Categories from the InfantRisk Center, which rates drugs from Level 1 (safest) to Level 5 (avoid).
- Level 1: No detectable transfer. Examples: insulin, heparin, most thyroid meds. Safe to use without worry.
- Level 2: Minimal transfer, no reported infant effects. Examples: sertraline, amoxicillin, ibuprofen, acetaminophen. These are the go-to choices.
- Level 3: Possible risk, monitor baby. Examples: fluoxetine, citalopram, diazepam. Use with caution, especially in newborns.
- Level 4: Possibly hazardous. Examples: lithium, cyclosporine. Only use if benefits clearly outweigh risks.
- Level 5: Contraindicated. Examples: radioactive iodine-131, chemotherapy drugs like methotrexate. Breastfeeding must stop.
Here’s the good news: 87% of commonly prescribed medications fall into Level 1 or 2. That means most of what you’re taking is fine. The American Academy of Pediatrics says only 1-2% of drugs are truly unsafe for breastfeeding. The rest just need smart timing or monitoring.
Some drugs are sneaky. High-dose estrogen birth control pills (over 50 mcg ethinyl estradiol) can slash your milk supply by 40-60% within three days. That’s why progestin-only pills are recommended. Bromocriptine? It shuts down milk production in 95% of women. Avoid unless you’re not planning to breastfeed.
When and How to Take Medications Safely
Timing your doses can cut your baby’s exposure by 30-50%. The best strategy? Take your medication right after you breastfeed. That gives your body 3-4 hours to clear most of the drug from your bloodstream before the next feeding.
For drugs with long half-lives-like diazepam or fluoxetine-this is even more important. If you take a 10 mg dose of diazepam, your baby could get a buildup over time. But if you take it after the evening feeding, your baby won’t get much during the overnight feed.
For antidepressants, doctors often recommend checking your baby’s blood levels at 2 weeks if you’re on a higher dose. Watch for signs like excessive sleepiness, poor feeding, or irritability. Studies show 8.7% of infants on SSRIs show irritability, and 5.3% have trouble feeding. These aren’t common, but they’re signals to pause and check.
If you’re getting a nuclear medicine scan-like a VQ scan with Tc-99m-you’ll need to pump and dump for 12-24 hours. But for an FDG-PET scan? You can keep breastfeeding. Only 0.002% of the dose ends up in milk. That’s practically nothing.
Why So Many Moms Stop Breastfeeding Over Medication Fears
Here’s the sad part: 42% of U.S. mothers stop breastfeeding before six months. Medication concerns are the third most common reason-after perceived low milk supply and nipple pain. And here’s the twist: 15-30% of those mothers stop even though the drug they’re taking is safe.
Why? Because misinformation spreads fast. A doctor might say, “We’re not sure,” and the mom hears, “Don’t do it.” Or a friend says, “I took X and my baby got sick,” even if it was a coincidence. The result? Unnecessary weaning.
But data shows otherwise. A 2022 study found that 56.3% of breastfeeding women take medications. Only 12.7% are using ones classified as risky. And in most cases, the baby shows no symptoms. The real danger isn’t the drug-it’s the fear.
That’s why tools like the InfantRisk Center’s LactMed app (version 3.2, updated January 2023) are so important. It uses 12 pharmacokinetic factors to give you a real-time safety rating. No guesswork. Just facts.
What You Should Do Right Now
If you’re breastfeeding and need medication:
- Don’t stop breastfeeding without checking. Most drugs are safe.
- Ask your doctor or pharmacist: “Is this safe for breastfeeding?” and ask for the Lactation Risk Category.
- Take your dose right after feeding, not before.
- Watch your baby for changes in sleep, feeding, or mood-especially in the first two weeks.
- Use trusted resources like the InfantRisk Center or LactMed app, not random websites.
Remember: breastfeeding is one of the most protective things you can do for your baby. Stopping because of a medication you don’t need to stop for can do more harm than good. You’re not alone. Millions of moms take meds while breastfeeding. With the right info, you can too.
Do all medications pass into breast milk?
No. Most medications pass in very small amounts, and some don’t pass at all. Drugs with high molecular weight (over 800 daltons), like heparin, or those that are highly protein-bound, like warfarin, barely enter breast milk. Only about 1-2% of medications are considered unsafe for breastfeeding.
Is it safe to take antidepressants while breastfeeding?
Yes, many are. Sertraline is the most commonly prescribed and has the lowest transfer rate-only 1-2% of the mother’s dose reaches the baby. It’s rated Level 2 by the InfantRisk Center. Other SSRIs like fluoxetine are higher risk due to longer half-lives. Always monitor your baby for irritability or poor feeding, and check levels if you’re on a high dose.
Can I take painkillers like ibuprofen or acetaminophen while breastfeeding?
Absolutely. Both ibuprofen and acetaminophen are Level 1 medications. They transfer in tiny amounts-less than 1% of your dose-and have no known effects on infants. They’re among the safest options for pain or fever while breastfeeding.
What about birth control pills? Can I use them while breastfeeding?
Progestin-only pills are safe and won’t affect milk supply. But pills containing high-dose estrogen (over 50 mcg ethinyl estradiol) can reduce milk production by 40-60% within 72 hours. Avoid combination pills in the first 6 weeks postpartum, and consider progestin-only options or non-hormonal methods.
How do I know if my baby is affected by a medication in my milk?
Watch for changes in behavior: excessive sleepiness, poor feeding, fussiness, or unusual crying. For antidepressants, irritability affects about 8.7% of infants. If you notice these signs, contact your pediatrician. They can check your baby’s medication levels if needed. Most babies show no symptoms at all.
Should I pump and dump after taking medication?
Only if your doctor says so. For most medications, pumping and dumping isn’t necessary. The drug clears from your blood naturally over time. Taking the medication right after feeding is more effective than pumping. Exceptions include radioactive iodine or certain chemotherapy drugs-those require temporary interruption.
Are herbal supplements safe while breastfeeding?
Not necessarily. Herbal products aren’t regulated like prescription drugs, so their safety data is limited. Some, like fenugreek, may increase milk supply but can cause allergic reactions in babies. Others, like kava or goldenseal, may be harmful. Always check with your provider before using any supplement.
So many moms panic over meds when the science is actually super reassuring. I had to take sertraline after my second kid and was terrified-turned out my little one was sleeping better than ever. The key is knowing your drug’s category and timing doses right. This post nailed it.
Thank you for this meticulously researched piece. The distinction between passive diffusion and ion trapping is rarely explained so clearly. I’m an Indian pharmacist, and I’ve seen too many mothers discontinue breastfeeding due to misinformation. LactMed is indispensable-please share it widely.
While the data presented is largely accurate, one must consider the variability in infant metabolism. A 2021 meta-analysis in the Journal of Perinatal Pharmacology showed that neonates with CYP2D6 ultra-rapid metabolizer phenotypes may process SSRIs differently, leading to unpredictable serum levels-even with low transfer rates. Monitoring remains essential, regardless of category.
Let’s be real-doctors say ‘it’s safe’ like it’s a free pass. Meanwhile, I know a woman whose baby developed a rash after she took ibuprofen. Coincidence? Maybe. But now she’s on a 12-page spreadsheet tracking every pill, every feeding, every burp. And honestly? I get it. The system’s not built for moms who want certainty, not just statistics.
Wow. So much text. I skimmed. I’m just here to know if Advil is okay. Is it?
Of course you’re telling people it’s fine. You’re not the one holding a screaming infant at 3 a.m. wondering if the Zoloft is making them twitch. The real danger isn’t the drug-it’s the guilt you feel when you realize you trusted a blog over your gut.
The entire premise assumes that biological transfer equals biological harm. But what if the real issue isn’t pharmacokinetics, but epigenetic imprinting? We’ve seen in rodent models that even sub-therapeutic maternal SSRI exposure alters offspring stress response pathways. Is ‘safe’ just a euphemism for ‘we haven’t measured the long-term cost yet’?
Man, I wish I’d had this when I was nursing my twins. I was taking amoxicillin for a sinus infection and spent three days crying because I thought I was poisoning them. The truth? My kids were fine. The fear? That’s what nearly broke me. This post is a gift. Please, share it with every new mom you know.
the whole thing is a big pharma scam to keep you on pills and make you feel guilty for not breastfeeding. heparin dont get in milk? sure buddy. and why do they never mention the 2018 study where babies of moms on antidepressants had higher rates of autism? oh right because the journal got defunded. dont trust the system
To the person who said ‘trust your gut’-I hear you. But your gut is screaming because you’ve been bombarded with fear for years. I had to choose between my mental health and my baby’s health. I chose my baby. Turns out, my baby needed a present, calm mom more than a perfectly drug-free breast. This post didn’t just inform me-it freed me.