
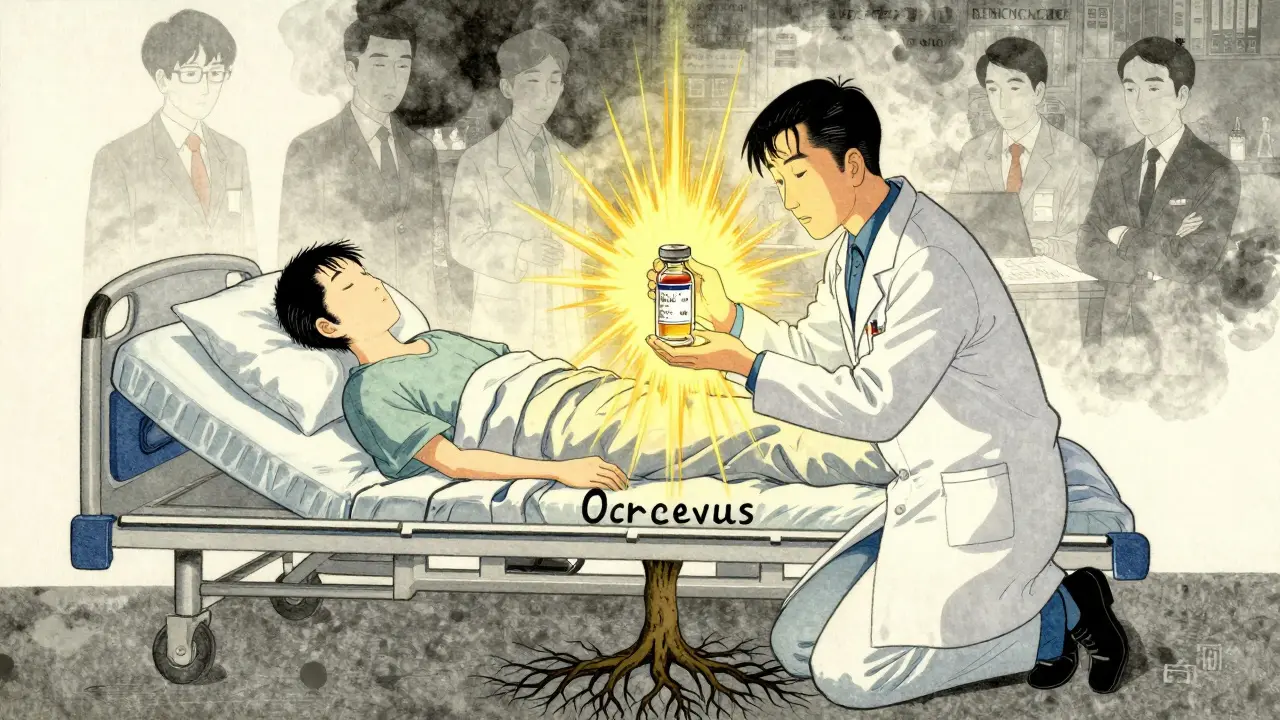
When a rheumatologist prescribes Humira instead of a biosimilar, or an oncologist insists on Ocrevus over a cheaper alternative, it’s not because they’re ignoring cost. It’s because the stakes are higher than most people realize. Specialty drugs aren’t just expensive-they’re complex, critical, and often the only option left for patients with rare or severe conditions. And when specialists choose brand-name drugs, it’s rarely about profit. It’s about survival.
The Real Cost of Specialty Drugs
Specialty drugs are defined by more than just price. The Centers for Medicare & Medicaid Services (CMS) sets the threshold at $670 per month, but most exceed $100,000 a year. These aren’t your typical pills you pick up at the corner pharmacy. They’re injectables, infusions, and biologics used for conditions like multiple sclerosis, rheumatoid arthritis, cancer, and rare genetic disorders. In 2021, these drugs made up just 6.2% of all prescriptions but accounted for 71.1% of total pharmacy spending. That’s a 75-fold difference in cost per patient compared to regular medications.It’s not just the price tag. These drugs require special handling-refrigeration, precise dosing, monitoring for side effects. Many need trained nurses to administer them. Patients need ongoing education. Pharmacies need certification. And the supply chain? Controlled tightly by just three pharmacy benefit managers (PBMs): CVS Caremark, Express Scripts, and OptumRx. Together, they handled 68% of specialty drug dispensing revenue in 2023.
Why Generics Don’t Always Work
You’ve heard the argument: generics are cheaper, just as effective. But with specialty drugs, that’s not always true. Take biosimilars-these are the closest thing to generics for biologic drugs. They’re designed to mimic the original, but they’re not identical. For patients with autoimmune diseases like Crohn’s or psoriasis, even small differences in how the drug behaves in the body can mean the difference between remission and flare-ups.One patient on Reddit shared how her Humira copay jumped from $50 to $850 when her insurance switched formularies. Her rheumatologist told her: biosimilars aren’t appropriate for her specific disease profile. That’s not anecdotal. A 2023 Medscape survey found that 79% of rheumatologists and 82% of oncologists say prior authorization delays and formulary restrictions directly impact their ability to choose the best drug for their patient. These aren’t bureaucratic hurdles-they’re life-or-death delays.
The Prescriber’s Dilemma
Doctors don’t wake up wanting to write expensive prescriptions. But they’re caught between two systems: one that demands cost control, and another that demands clinical precision. The American Medical Association reports physicians spend 13.4 hours a week just on prior authorizations-78% of that time tied to specialty drugs. That’s over half a workday each week just fighting insurance companies instead of treating patients.And when a patient’s only effective treatment is a brand-name drug, the pressure mounts. If a specialist switches a patient to a biosimilar and the disease flares up, who’s liable? Who pays for the hospitalization? Who deals with the lost work time? The answer is rarely the insurer. It’s the patient. And the doctor.
Studies show prescribers who receive payments from drug companies prescribe brand-name drugs at higher rates. But even without financial incentives, many doctors stick with brands because they’ve seen the outcomes. In oncology, where survival rates can hinge on milligram precision, there’s little room for trial and error. A 2024 American Society of Clinical Oncology report found that 85% of oncology drug spending goes to specialty agents-because there’s often no alternative.

The PBM Problem
It’s not just manufacturers driving prices. The real financial distortion is happening behind the scenes. The Federal Trade Commission’s 2025 report revealed that PBMs were marking up specialty generic drugs by thousands of percent. For example, a drug that costs $50 to acquire might be billed to insurers at $1,200. That’s not a markup-it’s a tax on the system. And it’s not happening with ordinary generics. It’s happening with specialty drugs, where patients have no choice.These markups are why a patient might pay $1,200 a month for Ocrevus-even with insurance. The PBM gets paid a cut, the specialty pharmacy gets paid, the manufacturer gets paid. The patient? They’re left with the bill. And their doctor? They’re stuck explaining why the cheaper option isn’t available.
What’s Changing?
There are signs of change. The Inflation Reduction Act of 2022 gave Medicare the power to negotiate prices for some high-cost drugs. Drugs like Jakafi, Ofev, and Xtandi are already on the list. That could bring down costs for thousands of patients. The Centers for Medicare & Medicaid Services also proposed new rules in March 2025 requiring greater pricing transparency from PBMs-potentially exposing $7.3 billion in hidden markups.But these are band-aids on a wound that’s been bleeding for over a decade. The real fix? A system that rewards clinical outcomes over profit margins. One that lets doctors prescribe based on what works-not what’s easiest to get approved. One that stops punishing patients for having rare diseases.
What Patients Can Do
If you’re on a specialty drug and struggling with costs:- Ask your doctor about patient assistance programs. Nonprofits like NORD helped 45,000 people in 2023 get access to these drugs.
- Request a therapeutic equivalency review. Sometimes, switching to a biosimilar is possible with proper monitoring.
- Appeal denials. Many insurance companies reverse decisions after a formal appeal, especially with doctor support.
- Know your rights. The FTC’s 2025 report confirmed that PBMs can’t hide their markups forever. New rules are coming.
The Bigger Picture
Specialty drugs are here to stay. By 2028, they’ll make up 73% of global prescription drug spending. That’s not a trend-it’s a transformation. And as more drugs enter the market-2,700+ are in development, 45% targeting rare diseases-the pressure on the system will only grow.But the question isn’t whether we can afford these drugs. It’s whether we can afford not to use them. For patients with no other options, brand-name drugs aren’t a luxury. They’re a lifeline. And when specialists choose them, it’s not because they’re biased. It’s because they’ve seen what happens when the system fails.
The real issue isn’t brand preference. It’s a system that lets pricing be dictated by middlemen, not medicine.
Why do specialists prefer brand-name drugs over generics?
Specialists often choose brand-name drugs because many specialty conditions-like multiple sclerosis, certain cancers, or rare autoimmune diseases-have no proven alternatives. Biosimilars may be similar, but not identical, and switching can lead to disease flare-ups or loss of effectiveness. For patients who’ve already tried generics without success, the brand is the only option that works.
Are brand-name specialty drugs really that much more expensive than generics?
Yes-dramatically so. While generics make up 90% of prescriptions, they account for only 17.5% of total drug spending. Specialty brand-name drugs, by contrast, represent just 1-2% of prescriptions but over half of all drug spending. One patient on a specialty drug may cost $38,000 a year, compared to $492 for a typical medication. That’s a 75-fold difference.
Do pharmaceutical companies influence doctors’ prescribing habits?
Yes, but it’s not the whole story. ProPublica found doctors who received over $5,000 from drug companies in 2014 prescribed brand-name drugs at rates 50% higher than those who received nothing. But even without payments, many specialists choose brands because they’ve seen better outcomes. Clinical experience often outweighs financial incentives.
Why can’t insurance just cover the cheaper option?
Insurance plans often block cheaper drugs through formularies and prior authorizations. But when a doctor argues the generic won’t work for a specific patient, insurers are required to review. The problem? The process takes weeks, and delays can cost patients their health. Some insurers also benefit from PBM markups on brand-name drugs, creating a financial incentive to keep them on the list.
What’s being done to lower specialty drug prices?
The Inflation Reduction Act allows Medicare to negotiate prices for certain high-cost drugs, starting with 10 in 2026. New CMS rules in 2025 will require PBMs to disclose markups on specialty drugs. Congress is also considering the Specialty Drug Price Transparency Act, which would cap PBM profits. These are early steps, but they’re the first real attempts to fix a broken system.
How can patients reduce their out-of-pocket costs?
Patients can apply for manufacturer assistance programs, nonprofit aid (like NORD), or patient copay cards. Many specialty pharmacies offer financial counseling. Always ask your doctor for help-many have relationships with these programs. Also, appeal denials. Nearly 40% of appeals succeed when backed by clinical documentation.
This is why canada needs to stop letting american pharma run our health system. These drugs cost 3x here and we still get screwed. My cousin got denied humira for 8 months because some PBM in minnesota decided her 'case wasn't urgent enough'. Fuck that.
I appreciate the depth of this analysis. It is truly alarming how systemic inefficiencies are directly impacting patient survival. The administrative burden on physicians is not merely inconvenient-it is ethically untenable. We must advocate for policy reform that prioritizes clinical judgment over corporate profit margins.
Let me get this straight-doctors are the heroes here? Meanwhile, the same people who prescribe these $100k drugs are the ones who won’t even prescribe antibiotics for a sinus infection without a CT scan. This isn’t about survival. It’s about fear of liability wrapped in a white coat.
You think this is bad? Try living in a country where you have to file 17 forms just to get a prescription filled... and then your insurance says 'sorry, we don't cover that biologic because it's not on our 'preferred' list'... like it's a damn Netflix subscription. PBMs are the real villains here. Not doctors. Not patients. The middlemen who get rich while you die waiting.
I have a friend with lupus who switched to a biosimilar and ended up in the ER with a full flare-up. She cried for days because she couldn't afford to go back to the brand. I just want people to understand-this isn't about 'choice'. It's about survival. 💔
Ah yes, the classic 'doctors are saints' narrative. Let’s not ignore the fact that 60% of rheumatologists receive consulting fees from AbbVie. The system is rigged. And yes, I know you’ll say 'but they’ve seen the outcomes'-so have I. Outcomes for shareholders, not patients.
I used to work in a specialty pharmacy. Saw it all. Patients crying because they had to choose between insulin and their biologic. Doctors writing letters so thick they needed a forklift to deliver them. The system doesn't care if you live or die. It only cares if the invoice clears. 😔
This is why I hate 'compassionate' liberals. They cry about patients but never question why we let pharma CEOs make $200M a year while people ration insulin. It’s not the PBM’s fault-it’s the whole capitalist cancer that turns medicine into a commodity. Fix the system or shut up.
My dad’s on a specialty drug. He pays $100 a month because his VA covers it. I wish everyone could have that. Why do some people get a lifeline and others get a bill they can’t pay? It ain’t fair.
In india we dont even have access to these drugs. My cousin with RA is on methotrexate and steroids. She cries every month because she cant afford the real stuff. So dont talk about biosimilars here. We dont even have the basics.
I’m not saying doctors are evil. But when your life depends on a drug that costs more than a Tesla, and the only people who benefit are the ones who never even met you... isn’t that just moral laziness dressed up as 'clinical expertise'?
I just got my insurance letter saying they're switching me to a biosimilar. My doctor said 'I know you're scared, but we'll monitor you.' But what if I flare? Who pays for my missed work? My rent? My therapist? Nobody. So I'm just supposed to trust them?
Wait so if I understand correctly... the drug company makes it, the PBM marks it up 20x, the pharmacy gets a cut, the doctor gets pressured, and the patient gets stuck with the bill? 😳 That’s not a healthcare system. That’s a pyramid scheme.