
Asthma Medication Comparison Tool
Find Your Best Asthma/COPD Medication
Answer a few questions to get personalized medication recommendations based on your priorities.
Your Priorities
If you or someone you care for is fighting asthma or COPD, you’ve probably seen the name Quibron‑T on a prescription bottle. But how does it stack up against other inhaled or oral treatments? This guide walks through the science, the pros and cons, and the real‑world costs so you can decide whether Quibron‑T is the right fit or if another option makes more sense.
Quick Takeaways
- Quibron‑T is a branded oral form of theophylline, a methylxanthine bronchodilator that works by relaxing airway smooth muscle.
- It is cheaper than many newer inhalers but has a narrow therapeutic window, requiring blood‑level monitoring.
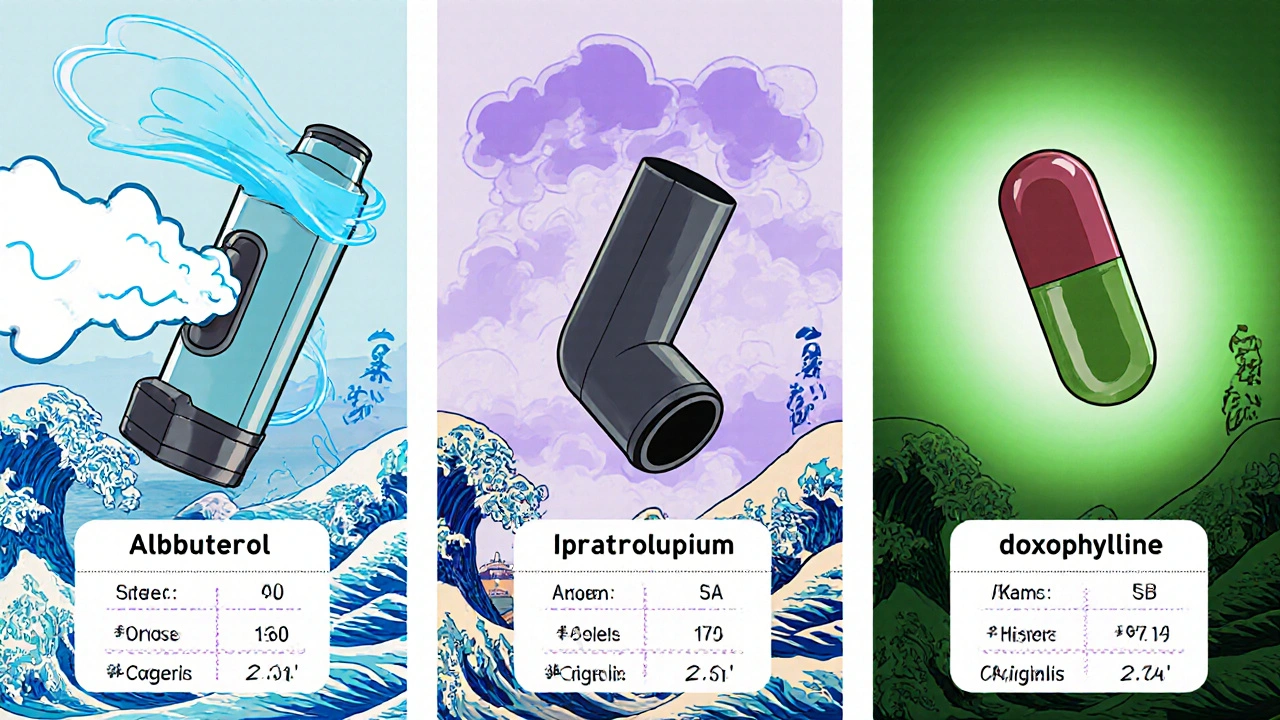
- Alternative bronchodilators like albuterol, ipratropium, and doxophylline offer faster onset or fewer side effects, but often cost more.
- Choosing the best medication depends on disease severity, lifestyle, cost tolerance, and how well you tolerate side effects.
- Regular review with your pharmacist or doctor is essential, especially when adding new drugs that could interact with theophylline.
What Is Quibron‑T?
Quibron‑T is a tablet formulation of theophylline approved for chronic asthma and chronic obstructive pulmonary disease (COPD). The brand contains 200 mg of theophylline per tablet and is taken once or twice daily depending on the prescribed dose.
How Theophylline Works
Theophylline belongs to the methylxanthine class. It inhibits phosphodiesterase, raising cyclic AMP levels in airway smooth muscle. This leads to relaxation of the bronchi and improves airflow. It also has mild anti‑inflammatory effects and can increase the force of diaphragmatic contraction.
Because its therapeutic range is narrow (typically 10‑20 µg/mL in blood), clinicians often order periodic serum level checks to avoid toxicity, which can cause nausea, tachycardia, or seizures.
Popular Alternatives to Quibron‑T
Below are the most common drugs patients consider when looking for a theophylline substitute.
Albuterol is a short‑acting β2‑agonist (SABA) inhaler that provides rapid relief of bronchospasm. It works within minutes and lasts 4‑6 hours.
Ipratropium is an anticholinergic inhaler that blocks muscarinic receptors, reducing mucus secretion and bronchoconstriction. It is often used twice daily for maintenance.
Doxophylline is a newer methylxanthine analogue that offers similar bronchodilation with fewer cardiac side effects and a wider therapeutic window.
Montelukast is a leukotriene‑receptor antagonist taken orally once daily. It helps with allergic asthma and reduces the need for steroids.
Salmeterol is a long‑acting β2‑agonist (LABA) inhaler, usually combined with an inhaled corticosteroid for maintenance therapy.
Roflumilast is a phosphodiesterase‑4 inhibitor taken orally once daily for severe COPD; it reduces inflammation rather than providing immediate bronchodilation.
Side‑Effect Profiles at a Glance
- Theophylline (Quibron‑T): nausea, headache, insomnia, arrhythmia, drug‑interaction risk.
- Albuterol: tremor, tachycardia, anxiety; generally well‑tolerated for short‑term use.
- Ipratropium: dry mouth, cough, rare urinary retention.
- Doxophylline: similar to theophylline but milder cardiac effects.
- Montelukast: mood changes, abdominal pain; minimal respiratory side effects.
- Salmeterol: risk of asthma‑related death if used without steroids; muscle cramps.
- Roflumilast: weight loss, diarrhea, depression.
Cost Comparison (NZD Approx.)
| Medication | Drug Class | Typical Dose | Onset | Duration | Common Side Effects | Monthly Cost (NZD) |
|---|---|---|---|---|---|---|
| Quibron‑T | Methylxanthine | 200 mg 1‑2×/day | 30‑60 min | 12‑24 h | Nausea, insomnia, arrhythmia | ≈ $15 |
| Albuterol (inhaler) | SABA | 90‑180 µg as needed | 1‑5 min | 4‑6 h | Tremor, tachycardia | ≈ $30 |
| Ipratropium (inhaler) | Anticholinergic | 2 puffs QID | 15‑30 min | 4‑6 h | Dry mouth, cough | ≈ $35 |
| Doxophylline | Methylxanthine analogue | 300 mg BID | 30‑60 min | 12‑24 h | Headache, mild GI upset | ≈ $25 |
| Montelukast | Leukotriene antagonist | 10 mg daily | 2‑4 h | 24 h | Mood changes, abdominal pain | ≈ $20 |
| Salmeterol (inhaler) | LABA | 50 µg BID | 15‑30 min | 12 h | Muscle cramps, rare cardiac events | ≈ $45 |
| Roflumilast | PDE‑4 inhibitor | 500 µg daily | 2‑4 h | 24 h | Weight loss, depression | ≈ $55 |
When Quibron‑T Might Be the Best Choice
Consider these scenarios:
- Cost‑sensitive patients: The tablet is inexpensive and covered by most NZ public health subsidies.
- Patients who struggle with inhaler technique: Oral dosing removes the need for correct inhaler coordination.
- Long‑term maintenance: Once‑daily or twice‑daily dosing fits a routine for chronic disease.
- Those already on multiple inhalers: Adding another inhaler could increase complexity and reduce adherence.

Potential Pitfalls and How to Mitigate Them
- Therapeutic drug monitoring: Schedule blood tests every 3‑6 months or after any new medication is introduced.
- Drug interactions: Theophylline is metabolized by CYP1A2; avoid concurrent fluoroquinolones, macrolide antibiotics, or cimetidine without dose adjustment.
- Smoking: Tobacco induces CYP1A2, lowering serum levels; smokers may need higher doses, but the risk of toxicity rises if they quit suddenly.
- Age considerations: Elderly patients have reduced clearance; start at the lower end of the dose range.
Making the Decision Together
Talk with your prescriber about:
- Frequency and severity of your symptoms.
- Any other medicines you take, especially antibiotics or antidepressants.
- Your budget and whether you qualify for government subsidies.
- Personal preferences: oral tablets vs. inhalers, once‑daily vs. multiple doses.
A shared decision‑making approach ensures you get a plan that balances effectiveness, safety, and affordability.
Frequently Asked Questions
What is the normal blood level range for theophylline?
Therapeutic levels are typically 10‑20 µg/mL. Values above 20 µg/mL increase the risk of nausea, seizures, and cardiac arrhythmias.
Can I use Quibron‑T and an albuterol inhaler together?
Yes. Theophylline provides long‑term control while albuterol offers rapid relief. Just keep the inhaler handy for breakthrough symptoms.
Why do I need blood tests for a tablet I take at home?
Because the therapeutic window is narrow, small changes in metabolism (e.g., from new drugs or smoking) can push levels into toxicity or sub‑therapeutic zones. Regular checks keep you safe.
Is doxophylline a safer version of theophylline?
Doxophylline shares the bronchodilator effect but has less impact on heart rate and fewer drug interactions, making it a good alternative for patients who experienced cardiac side effects on theophylline.
How quickly will I feel relief after taking Quibron‑T?
Onset is usually 30‑60 minutes, which is slower than inhaled rescue meds. That’s why it’s not used for sudden attacks.
Can I replace my inhaled steroids with Quibron‑T?
No. Theophylline does not control airway inflammation as effectively as inhaled corticosteroids. It’s typically added to, not substituted for, steroid therapy.
What should I do if I miss a dose of Quibron‑T?
Take it as soon as you remember, unless it’s almost time for the next dose. Then skip the missed one and continue with your regular schedule-don’t double‑dose.
By weighing the pros and cons above, you’ll be in a better position to discuss with your healthcare team whether Quibron‑T or another asthma/COPD medication best fits your life.
Hey folks, if you’re watching your budget but still need solid asthma control, Quibron‑T can be a real win. It’s cheap, taken as a simple tablet, and skips the hassle of mastering inhaler technique. For people who struggle with coordinating breaths, that oral route is a breath of fresh air. Just remember you’ll need occasional blood‑level checks, but that’s a small price for steady relief. Pair it with a rescue inhaler for those sudden flare‑ups and you’ve got a balanced plan. Keep the conversation open with your doctor and you’ll stay on top of any side‑effects.
The aether of modern pharmacology whispers that convenience outweighs nuance Yet theophylline’s narrow window reminds us that simplicity is a double‑edged sword Embrace the cheapness but do not neglect the spectral shadows of drug interactions Let the discourse be guided by both economics and biology
In the theater of breath, Quibron‑T takes the stage with a melancholy grace It promises relief while its serum levels dance on a razor’s edge The drama of nausea and insomnia haunts those who ignore the monitoring The allure of a low price hides a tempest of cardiac whispers Yet for the brave who tame it, the lungs sing a temporary lullaby Remember, every pill is a pact with the unseen forces of metabolism
For patients considering Quibron‑T, it is essential to evaluate both clinical efficacy and individual lifestyle factors. The medication offers an oral alternative that may improve adherence for those with inhaler technique challenges. However, regular therapeutic drug monitoring should be incorporated into the management plan to mitigate toxicity risk. Discuss with your healthcare provider how comorbid conditions and concurrent medications may influence dosing. An inclusive, shared‑decision approach ensures optimal outcomes for diverse patient populations.
What the pharmaceutical giants do not tell you about Quibron‑T is that its low price is not a benevolent act of generosity but a calculated maneuver to keep patients locked into a cycle of monitoring and repeat prescriptions.
The theophylline molecule, discovered over a century ago, has been repackaged in a glossy brand name that masks the truth about its narrow therapeutic window.
Every time you go for a blood test, the lab technicians collect data that feeds into databases owned by corporations who then use algorithms to adjust your dosage in ways that benefit their bottom line.
The alleged need for serum level checks is presented as a safety measure, yet the same labs are often the ones subsidizing the very drug they monitor.
If you look closely, you will see a pattern where newer inhalers with higher costs claim superior efficacy while the old‑school oral tablets are quietly promoted in public health subsidies.
This is not a coincidence; it is a strategic placement designed to divert attention from the fact that many newer agents have robust safety profiles and longer half‑lives.
Meanwhile, the myth of theophylline’s “quick bronchodilation” is propagated by outdated textbooks that have not been revised in decades.
The reality is that onset takes 30 to 60 minutes, making it unsuitable for acute attacks, a fact that is conveniently omitted in promotional leaflets.
Furthermore, the interaction profile of theophylline is a minefield, especially with common antibiotics and antidepressants, forcing patients to either endure side effects or switch drugs under doctor supervision.
The subtle pressure to stay on Quibron‑T becomes evident when you consider that smoking cessation abruptly raises serum levels, potentially leading to toxicity unless the dose is recalibrated.
Such recalibration requires an extra visit, an extra prescription, and ultimately a higher revenue stream for the healthcare system.
The narrative of cost‑effectiveness is also skewed because it fails to account for the indirect costs of monitoring, missed work days for appointments, and the anxiety patients experience while awaiting lab results.
In many countries, the government subsidizes Quibron‑T precisely because the pharmaceutical lobby argues that it reduces immediate medication expenses.
However, the long‑term economic burden, when you add the hidden monitoring fees and potential hospitalizations due to toxicity, tells a different story.
It is incumbent upon informed patients to question why a drug that requires such vigilance remains a first‑line recommendation in certain guidelines.
The answer, dear reader, lies in a web of profit incentives, regulatory inertia, and a healthcare system that sometimes rewards familiarity over innovation.
From a pharmacokinetic standpoint, Quibron‑T's bioavailability is fairly consistent, but the inter‑patient variability in CYP1A2 activity introduces a significant covariate in dose optimization. In clinical practice, integrating therapeutic drug monitoring (TDM) with population‑based Bayesian forecasting can streamline dose adjustments. The cost‑benefit analysis often hinges on the marginal utility of oral adherence versus inhaler technique barriers. Overall, the tablet remains a viable option for patients who prioritize convenience and have stable metabolic profiles.
Choosing a medicine that flirts with toxicity feels like a betrayal of one's own body. The so‑called “affordable” label should never excuse reckless side‑effects. Patients deserve treatments that respect their health, not just their wallets. When a drug forces you to watch your heart rate like a hawk you must ask where your safety truly lies. Moral responsibility belongs to developers and prescribers alike.
Quibron‑T is cheap but its monitoring headache outweighs the savings. Newer inhalers offer cleaner safety profiles. Stick to modern options unless budget is a major constraint.
Hey everyone, if you’re feeling stuck between cost and convenience, give Quibron‑T a look. It can be a solid backbone for maintenance when you pair it with a rescue inhaler. The key is staying on top of those blood levels – a quick check now and then keeps things smooth. Plus the oral route means no fiddling with spacers. Stay positive and keep the conversation open with your doc.
Honestly, theophylline feels like a relic you only see in old charts. Most patients will do better with a modern LABA plus steroid combo. The monitoring hassle just adds more work for the clinic. If you can afford it, skip the drama.
Push your limits, stay disciplined, and own your asthma regimen.