
Medication-Related Blood Clot Risk Calculator
Understanding Your Risk
This tool estimates your risk of developing blood clots due to medications based on factors discussed in the article. High risk requires immediate consultation with your healthcare provider.
Every year, tens of thousands of people develop dangerous blood clots not from injury or inactivity, but because of a medication they were prescribed. These aren’t rare accidents-they’re predictable, preventable reactions that often go unnoticed until it’s too late. If you’re taking birth control, hormone therapy, or cancer drugs, you’re at higher risk. And if you don’t know the signs, you could miss the warning signs until it’s an emergency.
What Medications Actually Cause Blood Clots?
Not all drugs cause clots, but some do-quietly, and without warning. The biggest culprits are medications that change how your blood behaves. Estrogen-based birth control pills, especially third-generation ones with desogestrel or gestodene, can raise your risk of a clot by 3 to 5 times compared to not taking them at all. Even over-the-counter hormone patches or rings carry the same risk. If you’re over 35 and smoke, that risk jumps even higher.Hormone Replacement Therapy (HRT)
For women going through menopause, HRT can ease hot flashes and night sweats-but it also increases clot risk by 2 to 3 times. That risk doesn’t stop at age 50. Women over 60 on HRT have the highest chance of developing a clot, especially if they’re overweight or have a history of migraines with aura.Cancer Treatments
Chemotherapy drugs like cisplatin and hormonal therapies like tamoxifen or androgen deprivation therapy for prostate cancer don’t just target tumors-they also make your blood stickier. People on these treatments are 4 to 7 times more likely to get a deep vein thrombosis (DVT) or pulmonary embolism (PE) than someone without cancer. The risk doesn’t disappear after treatment ends. It lingers for months.Other Risky Drugs
Some antibiotics, antidepressants, and even certain supplements like erythropoietin (used for anemia) can trigger clots. The FDA now requires black box warnings on all estrogen-containing medications, meaning the danger is officially recognized-and documented. But many patients still don’t know they’re at risk.How to Recognize a Medication-Induced Blood Clot
Symptoms don’t always come with a siren. They’re subtle. Often dismissed as muscle cramps, fatigue, or stress. But if you’ve started a new medication in the last 3 to 6 months and feel something off, don’t ignore it.Signs of Deep Vein Thrombosis (DVT)
- Swelling in one leg, usually the calf- Pain or tenderness that feels like a charley horse
- Skin that’s red, warm, or discolored
- A feeling of tightness or heaviness in the leg These symptoms usually appear on one side only. If both legs are swollen, it’s likely not a clot-but still worth checking.
Signs of Pulmonary Embolism (PE)
A clot that breaks loose and travels to your lungs is life-threatening. Symptoms include: - Sudden shortness of breath, even at rest- Sharp chest pain that gets worse when you breathe in
- Rapid heartbeat or palpitations
- Lightheadedness, dizziness, or fainting
- Coughing up blood If you have even one of these after starting a high-risk medication, get checked immediately. Don’t wait. Don’t assume it’s just anxiety or a cold.
How Doctors Diagnose These Clots
It’s not guesswork. There are clear tests doctors use to confirm a clot: - D-dimer blood test: Measures a substance released when clots break down. A negative result rules out a clot in low-risk patients. But if you’re on cancer therapy or have recent surgery, this test can be falsely positive. - Ultrasound: The go-to for checking leg veins. It’s non-invasive and accurate-but misses about 5-10% of clots, especially in the upper thigh or pelvis. - CT pulmonary angiogram: The gold standard for spotting clots in the lungs. It uses contrast dye and X-rays to map blood flow. It’s fast, but not always available in urgent settings. Doctors also use scoring systems to assess risk before symptoms appear. The Khorana Score is used for cancer patients. It looks at things like tumor type, platelet count, hemoglobin levels, and white blood cell count. A score of 2 or higher means you’re high risk-and should be on preventive medication.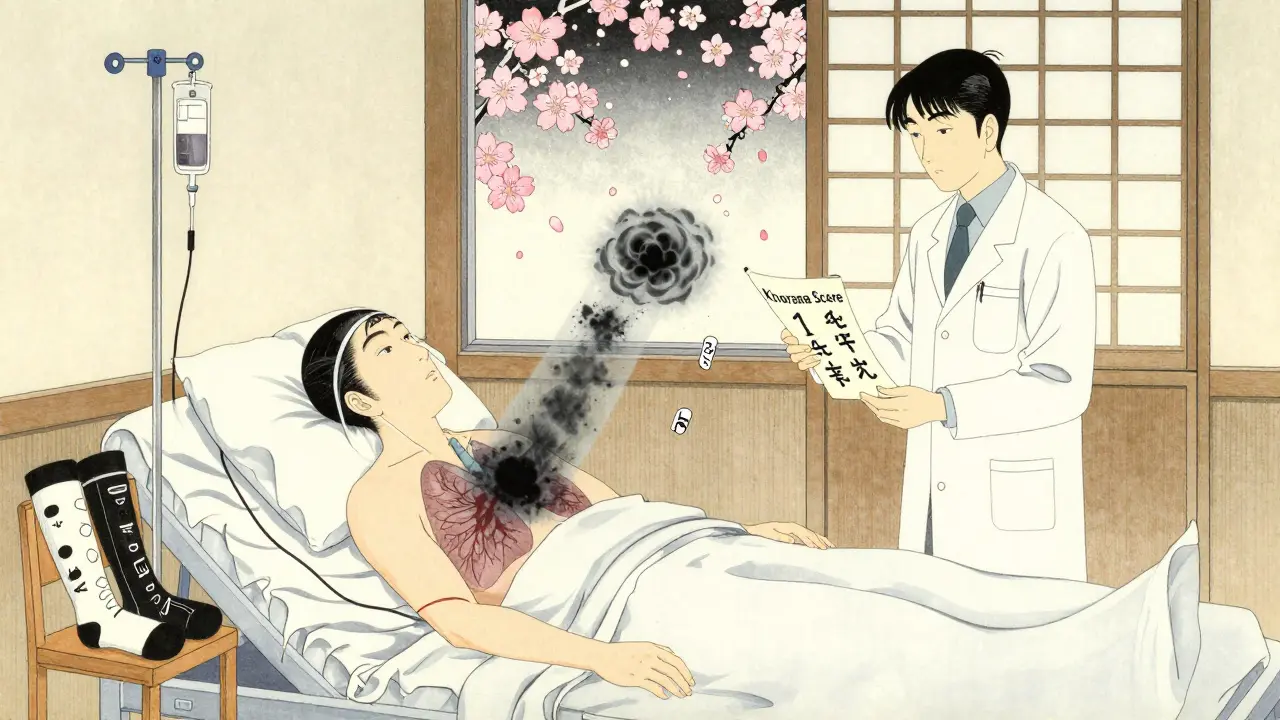
How to Prevent Blood Clots from Medications
Prevention isn’t optional. It’s essential. And it doesn’t mean stopping your treatment-it means managing the risk.Compression Stockings
If you’re hospitalized, recovering from surgery, or on long-term hormone therapy, compression stockings help. But they have to be fitted right. They need to provide 15-20 mmHg of pressure at the ankle, tapering off toward the thigh. Wearing them loosely? They’re useless. Wearing them too tight? They can cause skin damage. Replace them every 3-6 months-elasticity fades fast.Mechanical Devices
In hospitals, intermittent pneumatic compression devices are common. These inflatable cuffs wrap around your legs and squeeze every 10-15 seconds, mimicking muscle movement to keep blood flowing. They’re especially useful if you can’t walk after surgery.Anticoagulants: The Real Shield
For high-risk patients, drugs like enoxaparin (Lovenox) or DOACs like rivaroxaban and apixaban are the most effective prevention tools. Enoxaparin is given as a daily injection and cuts clot risk by 60-70%. DOACs are pills, easier to take, and don’t need blood tests. But they carry a slightly higher risk of bleeding-so they’re not for everyone.Travel and Daily Movement
Long flights, car rides, or even sitting at your desk for hours can trigger clots-especially if you’re on a risky medication. The CDC recommends: - Walking every 60-120 minutes during flights longer than 4 hours- Doing seated calf raises: lift your heels, hold for 3 seconds, lower. Repeat 10 times every 30 minutes
- Drinking 8-10 ounces of water every hour These simple steps can reduce travel-related clot risk by 30%.
Who Should Avoid Estrogen Completely?
If you have a known inherited clotting disorder-like Factor V Leiden or prothrombin gene mutation-you should never take estrogen-based medications. These conditions affect about 5% of white populations. Even if you’ve never had a clot before, the risk is too high. The same goes for antiphospholipid syndrome, where the clot risk jumps to 10-15% per year. That’s not a gamble. That’s a guarantee.Genetic Testing Is Available
Comprehensive panels can check for Factor V Leiden, protein C/S deficiency, and other mutations. Results take 5-7 days. If you’re planning to start birth control or HRT and have a family history of clots, ask your doctor about testing. It’s not routine-but it should be.
What to Do If You’re Already on a Risky Medication
Don’t panic. Don’t quit cold turkey. Talk to your doctor. Ask these questions: - Is this medication the best option for me?- What’s my personal clot risk based on my age, weight, and medical history?
- Should I be on a preventive anticoagulant?
- Do I need regular blood tests or scans?
- What symptoms should I watch for, and when should I go to the ER? If you’re a cancer patient, make sure your oncologist runs the Khorana Score at least once when you start treatment-and again every month. If you’re on HRT, get your blood pressure and liver function checked every 6 months. These aren’t just check-ups-they’re lifesavers.
The Bottom Line
Medication-related blood clots are not rare. They’re not random. They’re a known side effect of common treatments. And they’re preventable-if you know what to look for. You don’t need to avoid all medications. You just need to be informed. If you’re on birth control, HRT, or cancer therapy, talk to your doctor about your clot risk. Get tested if you have a family history. Wear compression stockings if you’re immobilized. Move your legs. Drink water. Know the symptoms. One missed sign can turn a routine prescription into a life-or-death emergency. Don’t wait for pain. Don’t wait for swelling. Ask questions before you start. Speak up if something feels wrong. Your life depends on it.Can birth control pills really cause blood clots?
Yes. Combined oral contraceptives containing estrogen increase the risk of blood clots by 3 to 5 times compared to not taking them. Third-generation pills with desogestrel or gestodene carry an even higher risk-1.5 to 2 times greater than older pills with levonorgestrel. The risk is highest in the first 3-6 months after starting and rises sharply if you’re over 35, smoke, or are overweight.
What should I do if I think I have a blood clot from my medication?
Don’t wait. If you have sudden leg swelling, chest pain, or shortness of breath after starting a new medication, go to the emergency room immediately. These could be signs of deep vein thrombosis (DVT) or pulmonary embolism (PE). Bring a list of your medications. Early diagnosis saves lives-delaying care increases the risk of death.
Are there natural ways to prevent medication-related clots?
Movement and hydration help, but they’re not enough on their own. Walking, calf exercises, and drinking water reduce risk-but if you’re on high-risk drugs like chemotherapy or estrogen therapy, you still need medical prevention like compression stockings or anticoagulants. Don’t rely on supplements like garlic, ginger, or omega-3s. They don’t replace proven treatments.
Can I switch to a safer birth control option?
Yes. Progestin-only pills, IUDs, implants, and condoms carry no increased clot risk. If you’re over 35, smoke, have a family history of clots, or have migraines with aura, switching to a non-estrogen method is strongly recommended. Talk to your doctor about alternatives that match your needs without the risk.
How long should I take anticoagulants after starting a risky medication?
It depends. For surgery or hospitalization, anticoagulants are usually given for 7-14 days. For cancer patients on long-term therapy, prophylaxis may continue for months or even years. For hormone therapy, most guidelines don’t recommend routine anticoagulants unless you have other risk factors. Your doctor will use your personal risk score to decide how long you need protection.
Let me guess-Big Pharma paid the FDA to slap on that 'black box warning' so they could sell you MORE expensive anticoagulants while you're still paying $200 a month for your 'life-saving' birth control. You think this is about health? No. It's about profit. They don't want you to know that natural alternatives like chasteberry, turmeric, and daily walking can do the same thing without the chemical cocktail. They need you dependent. They need you scared. And they need you buying pills-every. Single. Month.
My cousin took Yaz for three years. Never had a clot. Then she switched to 'safer' progestin-only-IUD? No. She got migraines, depression, and a 40-pound weight gain. Now she's on blood thinners for 'prevention.' Who's really being poisoned here? The system. Not the medication.
They tell you to get tested for Factor V Leiden-but they don't tell you that 90% of people with it NEVER get a clot. They're selling fear as medicine. And you're buying it. Hook, line, and syringe.
Why isn't anyone talking about how birth control was originally designed to control women's bodies-not their hormones? It's not medicine. It's social engineering. And now they're weaponizing clot risk to keep you compliant. You're not at risk because of desogestrel-you're at risk because you were never given a real choice.
And don't even get me started on 'compression stockings.' You know what they used to call those in the 1950s? 'Leg restraints.' Same thing. Just with better marketing.
Read the original studies. The 3-5x risk? That's compared to women who never took hormones. But what about women who smoke, sit all day, and eat fast food? Those are the real culprits. Blame the pill? Easy. Blame the system? Too hard.
I'm not saying don't be careful. I'm saying don't be manipulated. Question everything. Especially when the 'experts' all sound like they're reading from the same Big Pharma script.
And if you're still on estrogen? Good for you. You're brave. They'll call you reckless. But I'll call you free.
They want you afraid. Don't give them the satisfaction.
While I appreciate the emotional intensity of the previous comment, I must respectfully point out that the data on estrogen-containing contraceptives and clot risk is robust, peer-reviewed, and replicated across multiple large-scale epidemiological studies (e.g., the WHO Multinational Study, the Nurses’ Health Study). The 3–5x relative risk is not a marketing ploy-it's a statistical reality.
That said, absolute risk remains low: approximately 3–10 cases per 10,000 women per year, depending on age and smoking status. For context, pregnancy carries a 5–20x higher risk than birth control. And yes-movement, hydration, and avoiding smoking are critical mitigating factors.
Compression stockings? They’re not restraints. They’re evidence-based prophylaxis. And yes, they’re underutilized.
Anticoagulants aren't 'chemical cocktails'-they're life-saving interventions when indicated. The key is risk stratification, not fear-mongering.
So yes, question everything. But base your questions on science, not conspiracy.
And if you're over 35 and smoke? Please, for the love of all that is medically sound-quit smoking before you start a new pill. That’s the real villain here.
Let’s be real: this isn’t about scaring people. It’s about giving them back control.
I’ve seen too many patients panic when they hear 'blood clot'-then shut down and stop taking their cancer meds. Or worse-they keep taking their birth control, ignore the calf swelling, and show up in the ER three days later with a PE.
The goal isn’t to make you afraid. It’s to make you aware. Like knowing your car’s tire pressure matters before you hit the highway.
And yes-movement helps. But if you’re on tamoxifen and your legs feel like concrete after sitting for an hour? That’s not 'just tired.' That’s your body screaming.
Don’t wait for the siren. Listen for the whisper.
And if your doctor doesn’t run the Khorana Score? Ask again. Politely. But insist.
You’re not being paranoid. You’re being proactive.
And that? That’s the real power move.
In India, we have long understood that Western medicine over-medicalizes natural processes. Birth control is not a right-it is a corporate invention to control female fertility for profit-driven population engineering. The so-called 'risk' of clots is exaggerated to push expensive alternatives like IUDs and anticoagulants, which are often imported and unaffordable.
Our grandmothers never took pills. They ate turmeric, practiced yoga, and walked miles daily. Their blood flowed clean. Why do we now believe a synthetic hormone is safer than ancestral wisdom?
Moreover, the FDA’s black box warnings are meaningless when pharmaceutical companies fund medical education. The entire system is corrupted.
Indian women deserve access to traditional, holistic care-not patented chemicals disguised as science.
Stop trusting foreign regulators. Trust your body. Trust your culture.
And if you must take medication? Use the minimum dose for the shortest time possible. Never longer than necessary.
Our ancestors survived without pills. So can we.
Hey, I just started HRT last month and I was totally freaking out after reading this. But honestly? This post made me feel way less scared and way more ready to talk to my doctor. Like, I didn’t know about the Khorana Score or that compression socks need to be fitted right. I just thought 'oh, I’ll wear any socks.' 😅
Also-calf raises during Zoom calls? Yes. I’m doing them right now. My cat is judging me, but I don’t care.
Thank you for writing this. Not in a scary way. In a 'here’s what you can actually do' way. That’s rare.
Wow. So let me get this straight. You’re telling me that if I’m on birth control and I don’t want to die, I need to wear socks that cost more than my shoes, drink water like it’s my job, and possibly take blood thinners… just to sit at my desk and survive?
Meanwhile, my cousin in Cape Town just took the pill for 12 years, never had a clot, and still runs marathons. Meanwhile, I’m supposed to be terrified of my own hormones?
Look. I’m not denying risk. But this reads like a 50-page manual for anxiety.
Maybe the real issue isn’t the pill. Maybe it’s that we’re all sitting too much, eating processed food, and treating our bodies like machines that need constant maintenance.
Also-why is no one talking about how men on testosterone therapy have a 3x higher clot risk too? But we don’t get a 10-section blog post about it. Huh.
Anyway. I’ll do the calf raises. But I’m still taking my pill. And I’m not apologizing.
Okay, real talk: I was terrified after reading this. Like, heart-pounding, can’t-sleep terrified.
But then I called my OB-GYN. We talked. She ran my numbers. Turns out I’m low-risk: under 30, non-smoker, active, no family history. She said I’m fine on my current pill-and if I ever feel that 'tightness' in my leg? Just call. No shame.
This isn’t about panic. It’s about awareness. Knowledge is power. And you? You’re already ahead of 90% of people just by reading this.
Now go drink some water. Do a few calf raises. And breathe. You’ve got this.
I love how this post doesn’t just say 'here’s the danger'-it says 'here’s what you can DO.' That’s the difference between fear and empowerment.
I’m a nurse, and I’ve seen too many patients come in with PE because they thought 'it’s just a cramp' or 'my doctor didn’t mention it.' But here’s the thing: most doctors are overworked. They don’t have 20 minutes to explain clot risk to every patient on birth control.
So we have to be our own advocates. And this? This is the kind of info that helps.
Also-did you know that estrogen patches carry the same risk as pills? Most people think patches are 'safer.' They’re not. Same absorption. Same clot risk.
And if you’re on tamoxifen? The risk lingers for up to a year after stopping. That’s not common knowledge. Thank you for including that.
One more thing: if you’re traveling and you’re on any of these meds? Wear compression socks. Even if you think you’re 'fine.' I’ve seen too many 'fine' people end up in ICU.
Knowledge isn’t just power. It’s peace of mind.
If you’re on estrogen and feel one weird symptom, don’t wait-get checked.