Every year, over 150,000 people in the U.S. end up in the emergency room because something they ate messed with their medication. It’s not always obvious. Maybe you had a glass of grapefruit juice with your cholesterol pill. Or you ate a big salad with your blood thinner. These aren’t accidents-they’re preventable. The fix? A simple, personal food and medication interaction checklist you can make at home in under an hour.
Why Your Medication List Isn’t Enough
Most people keep a list of their pills: what they take, when, and why. That’s good. But it’s not enough. Medications don’t just interact with other drugs. They react with food, drinks, even vitamins and herbal supplements. And those reactions can be dangerous.Warfarin, for example, works to thin your blood. But if you eat a huge bowl of kale one day and none the next, your blood can clot-or bleed too much. Grapefruit juice can make statins 300% more powerful, leading to muscle damage. Dairy products can block antibiotics like ciprofloxacin from working at all. These aren’t rare cases. The FDA says 12% of all drug-related ER visits involve food or drink.
A checklist isn’t just a reminder. It’s a shield. Patients who use one have 37% fewer bad reactions, according to the American Pharmacists Association. And it’s not just for seniors. Nearly half of adults over 40 take three or more prescriptions. If you’re on any meds-especially blood thinners, antidepressants, heart meds, or antibiotics-you need this.
What Goes on the Checklist
A good checklist isn’t a scribble on a napkin. It’s a clear, organized record with five key parts for every medication:- Medication name (both brand and generic-like "Coumadin" and "warfarin")
- Dosage and schedule ("5 mg once daily at 8 AM")
- Purpose ("prevents blood clots")
- Prescribing doctor (name and clinic phone)
- Food/drug interactions (this is the core)
For interactions, don’t just say "avoid grapefruit." Be specific:
- High Risk - Avoid completely. Example: Grapefruit juice with simvastatin. This combo can cause muscle breakdown and kidney failure.
- Moderate Risk - Separate by time. Example: Dairy with ciprofloxacin. Wait at least 2 hours after taking the antibiotic before eating yogurt or cheese.
- Low Risk - Keep consistent. Example: Vitamin K in spinach with warfarin. Don’t avoid it-eat about the same amount every day.
Include exact amounts. "One cup raw spinach" is better than "greens." Cooking changes vitamin K levels by up to 70%. Raw kale affects your blood thinner differently than sautéed kale.
Where to Find Reliable Info
Don’t guess. Don’t trust random websites. Use trusted sources:- FDA Medication Guides - Every prescription comes with one. Look for the "Food and Drug Interactions" section.
- New Zealand Formulary Interaction Checker - Free, updated regularly, and used by pharmacists worldwide.
- SEFH Drug-Food/Herb Interaction Guide - A laminated card set you can stick on your fridge. Color-coded and easy to read.
- Your pharmacist - Ask them during your next refill. Most will review interactions for free.
Always write down where you got the info: "Per NZ Formulary, updated July 15, 2024." That way, if your doctor asks, you can show them the source.

Choose Your Format: Paper or Digital?
You’ve got options. Each has pros and cons.Paper Checklist - The FDA’s free "My Medicines" template works great. Print it, fill it out, and tape it to your fridge. It’s simple. No batteries. No login. In an emergency, paramedics can see it instantly. Over 90% of seniors over 75 use paper lists. If you’re not tech-savvy, this is your best bet.
Digital Apps - Apps like Medisafe and MyTherapy auto-check for interactions, send reminders, and sync with pharmacies. They’re great if you take five or more meds. A 2023 study found digital checklists cut errors by 42%. But they need a smartphone, Wi-Fi, and regular updates. If your phone dies, your checklist does too.
Best of both worlds? Print a paper copy and keep a digital version as backup. Or use laminated SEFH cards on your fridge and check your phone app weekly.
How to Build It (Step by Step)
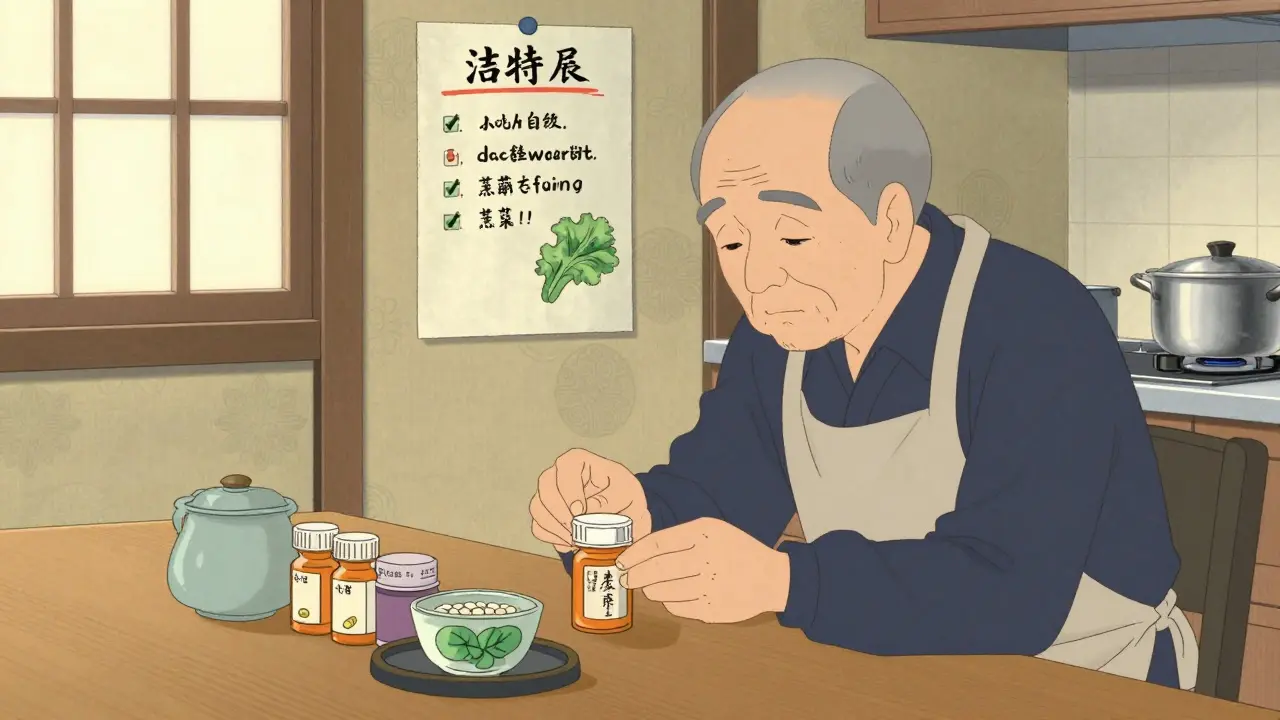
Step 1: Gather everything - Pull out every pill, capsule, patch, liquid, and supplement. Include OTC meds like ibuprofen, antacids, and vitamins. Put them on the table.Step 2: List each one - Write down the name, dose, time, and reason for each. Don’t skip the ones you take "only when needed."
Step 3: Research each interaction - Use the FDA guides or NZ Formulary. Look up each drug. Note the food, drink, or supplement it reacts with. Rate it High, Moderate, or Low Risk.
Step 4: Add emergency info - Two contacts (family or friend), your primary doctor’s number, and any known allergies (include reaction severity: "rash," "swelling," "trouble breathing").
Step 5: Date it and update it - Write the date you created it. Every time your meds change-new prescription, stopped drug, new supplement-update the checklist within 24 hours. Outdated lists cause 28% of errors.
What to Avoid
Don’t make these mistakes:- Using vague terms - "Avoid citrus" is useless. Say "avoid grapefruit, Seville oranges, pomelos."
- Ignoring supplements - St. John’s Wort can make birth control, antidepressants, and transplant drugs useless. It’s not "natural"-it’s powerful.
- Forgetting alcohol - It boosts sedatives, lowers blood pressure meds, and increases liver damage from acetaminophen.
- Not showing it to your doctor - Bring it to every appointment. Most doctors never ask. You have to lead.

Real-Life Wins and Warnings
One man on Reddit saved his kidney by writing down that grapefruit juice interfered with his tacrolimus (a transplant drug). He stopped drinking it after his checklist reminded him. He’s alive today because he wrote it down. Another person’s app warned her about kale with warfarin-but didn’t know she ate bok choy daily. Her levels dropped. She didn’t realize the problem until her doctor noticed. The key? Be specific. Know your food. Track it. Talk to your pharmacist.Keep It Alive
A checklist only works if you use it. Make it part of your routine:- Put it on the fridge or next to your pill organizer.
- Use red marker for high-risk items.
- Review it every time you refill a prescription.
- Ask your pharmacist to check it during your monthly medication therapy session.
Studies show patients who do this reduce errors by 65%. And if you’re on Medicare, these sessions are covered. No extra cost.
By 2026, most electronic health records will include your food-drug checklist. But right now, you have to build it yourself. It’s not hard. It’s not fancy. But it could save your life.
Can I just rely on my pharmacist to warn me about food interactions?
Pharmacists do their best, but they don’t know your full diet or daily habits. You might eat grapefruit every morning and forget to mention it. Or you might take a new supplement your pharmacist hasn’t seen yet. Your checklist is your personal record. It fills the gaps. Always bring it to the pharmacy-even if you think you don’t need to.
Do I need to avoid all foods that interact with my meds?
Not always. For high-risk items like grapefruit and statins, yes-avoid completely. For moderate ones, like dairy and antibiotics, separate them by 2 hours. For low-risk, like vitamin K and warfarin, consistency matters more than avoidance. Eat the same amount every day. Sudden changes are dangerous. Your checklist should explain why.
What if I don’t know the generic name of my medication?
Look at the pill bottle. The generic name is always listed. If it’s not clear, call your pharmacy. Or take a photo of the pill and use a free app like Drugs.com Pill Identifier. Don’t guess. Using the wrong name can lead to missed interactions. Accuracy saves lives.
Is it safe to use AI tools or apps that claim to check food-drug interactions?
Be careful. The FDA found 62% of unregulated AI apps give wrong or incomplete interaction info. Apps like Medisafe and MyTherapy are FDA-recognized and update regularly. Free apps from unknown developers? Don’t trust them. Use them only as a secondary check-not your primary source.
How often should I update my checklist?
Update it within 24 hours of any change: new prescription, stopped drug, added supplement, or even a new food habit (like starting daily green smoothies). Also, review it every 3 months. Your body, diet, and meds can change. Your checklist should too.
Can I use this checklist for my elderly parent?
Absolutely. In fact, it’s even more critical. Seniors often take 5+ medications. Paper checklists work best for them-no tech needed. Tape it to the fridge. Make the font large. Add color codes. Help them update it during their weekly pill sorting. A checklist can prevent hospital stays and even save their life.
Next Steps
Start today. Gather your meds. Print the FDA’s "My Medicines" template. Sit down for 45 minutes. Write it out. Talk to your pharmacist. Put it on the fridge. That’s it. You don’t need an app. You don’t need to be tech-savvy. You just need to act.Medication errors don’t happen because people are careless. They happen because systems assume you’ll remember. You won’t. But your checklist will. Make it. Use it. Protect yourself.
Okay, but let’s be real-how many of us actually *do* this? I’ve got a sticky note on my fridge that says ‘NO GRAPEFRUIT’ in glitter pen, and I still forgot last Tuesday. My pharmacist facepalmed. I’m not lazy-I’m just… creatively negligent. Maybe the checklist should come with a tiny bell you ring every time you take a pill. Or a song. Like, ‘Grapefruit juice is a traitor, don’t you dare!’
Oh, so now we’re all supposed to become pharmacists? My mom’s on 12 meds and can’t even remember her own birthday. You think she’s gonna write down ‘1 cup raw spinach = 70% less vitamin K than cooked’? This is why America’s healthcare is a circus. You want people to live? Fix the system. Not make them do your job.
Let’s be precise: the FDA doesn’t say ‘12% of all drug-related ER visits involve food or drink’-they say ‘approximately 12% of preventable adverse drug events in ambulatory care settings are associated with food-drug interactions.’ You’re conflating incidence with attribution. Also, ‘SEFH Drug-Food/Herb Interaction Guide’? That’s not a real product. It’s a fictional brand invented by a guy who runs a blog called ‘Herbal Truths.’ Don’t mislead people.
The elegance of this approach lies not in its complexity, but in its radical simplicity: a personal, tangible artifact of agency in a system designed to render us passive. To document one’s pharmacological ecosystem is to assert sovereignty over one’s corporeal autonomy. It is, in essence, an act of quiet rebellion against the commodification of health. One does not merely create a checklist; one composes a covenant with one’s own survival.
Hey, I just shared this with my dad who’s 78 and takes 6 pills every day. He said he’ll do it tomorrow. I printed the FDA template and put it on his fridge with a big red marker for the grapefruit thing. He didn’t even know grapefruit could mess with his blood pressure med. He’s not techy, so paper is perfect. Thanks for this! I think this could help so many people, especially in places where doctors don’t have time to explain everything. We just need to make it easy and normal to do this.
Just write down your meds and what to avoid. No fancy apps. No big words. If you take warfarin, don’t eat huge salads one day and none the next. If you take antibiotics, wait 2 hours after dairy. That’s it. Keep it simple. Your life is worth it.
Clear, practical, and evidence-based. A model of patient empowerment. The emphasis on source attribution and updating frequency is particularly commendable. This should be distributed by primary care networks as a standard template. Minimalist, effective, and scalable.
This is awesome! I showed this to my cousin who’s on antidepressants and she started using it last week. She said she finally feels in control. Even her mom, who’s super old-school, said ‘Huh. Maybe I should do this too.’ Small steps, big impact. Keep sharing stuff like this!
150,000 ER visits? That’s 0.04% of the U.S. population. The real issue is overprescribing. Pharma companies push drugs, doctors prescribe without context, and now we’re blaming food? This checklist is a Band-Aid on a hemorrhage. And who wrote the NZ Formulary? A Kiwi with a grudge against Americans? Also, ‘SEFH’ is not a real organization. It’s a phantom. This whole thing smells like a marketing campaign disguised as public health.
Oh, so now I need to become a clinical nutritionist with a laminated card and a color-coded system just to eat an avocado? How quaint. I suppose next you’ll ask me to log my emotional state before taking Prozac. ‘Mood: Existential dread. Interaction risk: High. Food consumed: Avocado toast. Outcome: Still alive.’ How poetic. How utterly, tragically human.
My uncle died from a grapefruit interaction. No one told him. He was 72. This checklist? It’s not a suggestion. It’s a lifeline. Do it. Now.