
Every year, millions of pregnant women reach for an OTC pill to ease a headache, soothe a cough, or calm heartburn. It feels harmless-after all, these are the same medicines you’ve used for years. But pregnancy changes everything. What was once a quick fix can become a hidden risk. The truth? OTC medications during pregnancy aren’t always safe, even if they’re on the shelf next to candy and gum.
You don’t need to panic. You don’t need to suffer in silence. You just need to ask the right questions before you swallow anything. Here’s what actually matters.
Is this medication even necessary?
Before you open the medicine cabinet, pause. Ask yourself: Do I really need this? Many pregnancy symptoms-like mild nausea, occasional headaches, or a stuffy nose-are temporary. They’re your body adjusting, not a problem needing a drug fix.
For example, heartburn? Try eating smaller meals, staying upright after eating, or sleeping with your head slightly elevated. A stuffy nose? Use a saline spray or a humidifier. These simple fixes work better than you think-and carry zero risk.
Medication should be your last resort, not your first instinct. If symptoms are mild, give your body time. If they’re getting worse, talk to your provider before reaching for a bottle.
What’s the lowest dose that works?
More isn’t better. In pregnancy, the goal isn’t to crush symptoms-it’s to manage them with the least amount of medicine possible.
Take acetaminophen (Tylenol). It’s still the go-to pain reliever during pregnancy, and for good reason. But even acetaminophen has limits. The maximum safe dose is 4,000 mg per day. That’s six 500 mg tablets. Taking eight, ten, or more because you’re in pain? That’s dangerous. High doses over time have been linked to possible developmental issues in babies, even if the evidence isn’t final yet.
Same goes for cold medicines. A single dose of dextromethorphan (plain Robitussin) is fine. But if you’re taking three different cold products at once-each with acetaminophen, dextromethorphan, and antihistamines-you’re accidentally overdosing. Always check labels. Look at the active ingredients. Don’t stack.
How long will you be taking it?
Short-term use is usually low-risk. Long-term use? That’s where things get tricky.
NSAIDs like ibuprofen (Advil, Motrin) and naproxen (Aleve) are okay for a day or two early in pregnancy-but not after 20 weeks. After that, they can cause serious problems: low amniotic fluid, kidney damage in the baby, and even heart complications. The FDA made this warning official in 2020, and drug labels changed to match.
Even acetaminophen isn’t risk-free if used daily for weeks. A major study tracking 50,000 pregnancies is still underway to see if long-term use affects brain development. Until we know for sure, the rule is simple: use it only when needed, for the shortest time possible.
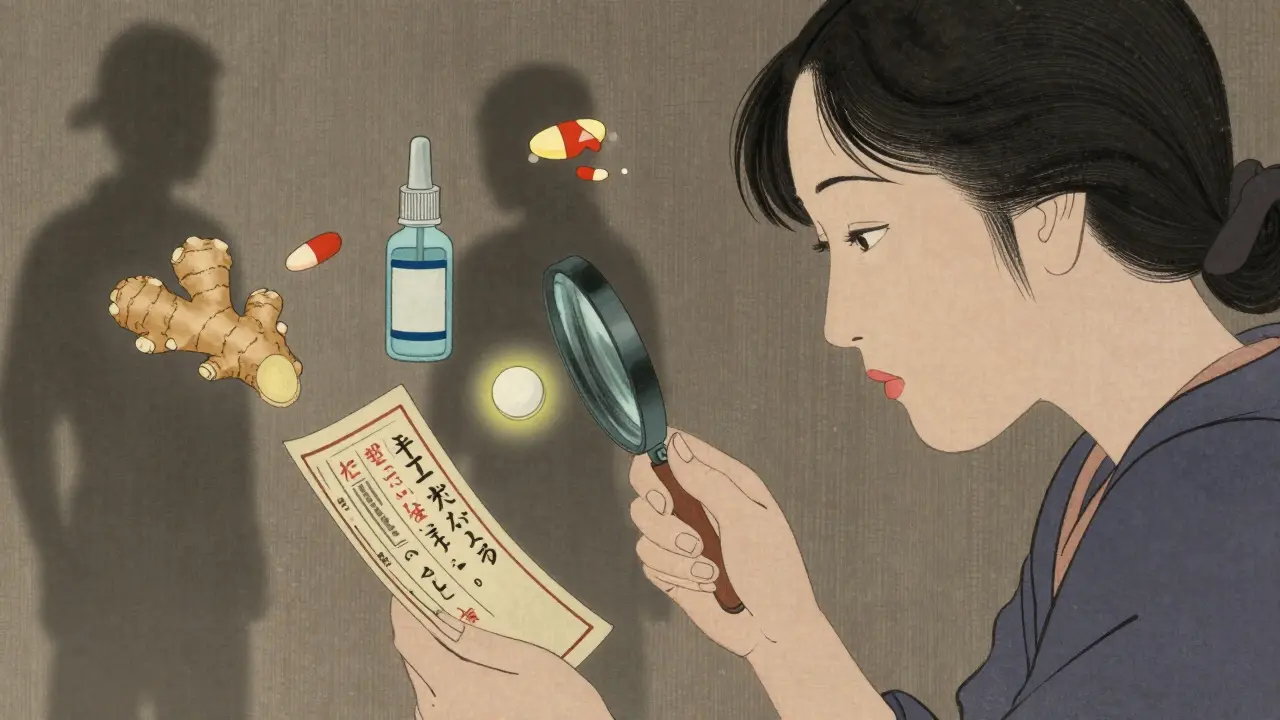
Are there non-drug options?
There’s a whole world of safe, natural ways to manage symptoms that don’t involve pills at all.
For nausea: Ginger tea, crackers before getting out of bed, or acupressure wristbands help more than most people realize.
For allergies: Loratadine (Claritin) and cetirizine (Zyrtec) are considered safe, but saline nasal rinses or avoiding allergens (like dust or pet dander) can cut symptoms without any medicine.
For constipation: Drink more water, eat more fiber (prunes, oats, beans), and move your body. A daily walk does more than a laxative.
For back pain: Prenatal yoga, physical therapy, or a supportive belly band often work better than painkillers.
These aren’t just "natural" alternatives-they’re often more effective and completely risk-free.
Has your provider approved this exact product?
This is the question most women skip. And it’s the most important one.
Not all "cough syrups" are the same. "Plain Robitussin" contains only dextromethorphan-and it’s safe. But "Robitussin Multi-Symptom Cold"? It has acetaminophen, phenylephrine, and guaifenesin. Phenylephrine is a decongestant linked to birth defects if used early in pregnancy. So you’re not just taking a cough medicine-you’re taking three drugs in one, and you didn’t even know it.
Same with antacids. Tums (calcium carbonate) is safe. But some other brands mix in aluminum or magnesium that can cause side effects. Always check the label. Write down the brand name and exact ingredients. Bring it to your next appointment.
And never assume "natural" means safe. Herbal teas, supplements, and essential oils? Many have no safety data in pregnancy. Some can trigger contractions or affect fetal development. Stick to what’s been studied-nothing else.
What about the first trimester?
The first 12 weeks are when your baby’s organs are forming. That’s the most sensitive time. Even small exposures can matter.
Decongestants like pseudoephedrine (Sudafed) are a big no-no in the first trimester. Studies show they can double the risk of rare birth defects like gastroschisis, where the baby’s intestines develop outside the body.
Diphenhydramine (Benadryl) is often used for sleep or allergies, but it’s not the best choice. It can cause drowsiness in both mom and baby, and there’s some evidence it might affect fetal movement. Better options? Loratadine or cetirizine-both are second-generation antihistamines with clean safety records.
And while acetaminophen is still the top pick for pain, don’t use it daily just to be safe. Use it only when you really need it.

What to do right now
You don’t need to wait for your next appointment. Start today.
- Make a list of every OTC medicine, supplement, or herbal product you’ve taken in the last 3 months. Include brand names and doses.
- Check your medicine cabinet. Throw out anything with pseudoephedrine, naproxen, or ibuprofen if you’re past 20 weeks.
- Write down the five questions from this article. Ask them every time you consider taking something new.
- Call your provider with your list. Don’t wait. Even if you think it’s "just a cold."
Most providers will tell you they discuss OTC safety at the first prenatal visit. But 32% of pregnant women still start OTC meds without asking anyone. Don’t be one of them.
What’s changing in 2026?
Science is catching up. In 2023, researchers found that 23% of pregnant women have a gene variation that changes how their body breaks down acetaminophen. That means the "safe" dose of 4,000 mg might be too much for some-and too little for others.
Future guidelines may include genetic testing to personalize OTC advice. But that’s still years away. Right now, the best tool you have is awareness.
The bottom line? No OTC medication is 100% safe in pregnancy. But with the right questions, you can avoid the risks and still feel better.
Is Tylenol safe during pregnancy?
Yes, acetaminophen (Tylenol) is still considered the safest pain reliever during pregnancy when used as directed. The maximum daily dose is 4,000 mg. Avoid taking it daily for weeks at a time, and never combine it with other cold or pain medicines that also contain acetaminophen. While some new research is looking at possible links to neurodevelopmental effects, major medical groups still recommend it as the best option for short-term use.
Can I take ibuprofen while pregnant?
No, after 20 weeks of pregnancy. Ibuprofen and other NSAIDs can cause serious problems for the baby, including low amniotic fluid and kidney damage. Even before 20 weeks, they may increase the risk of miscarriage. Avoid them completely unless your doctor specifically says otherwise. Use acetaminophen instead for pain or fever.
What cold medicines are safe during pregnancy?
Stick to single-ingredient products: plain Robitussin (dextromethorphan only) for cough, saline nasal spray for congestion, and acetaminophen for fever or headache. Avoid multi-symptom cold remedies-they often contain decongestants like phenylephrine or pseudoephedrine, which are unsafe, especially in the first trimester. Always read the label. "Plain" is key.
Is Benadryl safe for allergies during pregnancy?
It’s not the best choice. Benadryl (diphenhydramine) can cause drowsiness in both you and your baby, and it may affect fetal movement. Better options are loratadine (Claritin) or cetirizine (Zyrtec), which are non-drowsy and have strong safety data. If you’ve been using Benadryl regularly, talk to your provider about switching.
Are herbal remedies safe during pregnancy?
Most aren’t proven safe. Herbal teas, supplements, and essential oils aren’t regulated like medications, and many haven’t been tested in pregnancy. Some, like black cohosh or goldenseal, can trigger contractions. Others, like peppermint tea, are fine in small amounts-but don’t assume "natural" means safe. Always check with your provider before using anything herbal.
Should I stop all OTC meds during the first trimester?
Not necessarily-but be extra cautious. The first trimester is when your baby’s organs form, so avoid anything unnecessary. If you need something, choose the safest option (like acetaminophen or Claritin) and use the lowest dose for the shortest time. Never start a new OTC medicine without talking to your provider first.
What if you already took something risky?
If you took ibuprofen after 20 weeks, or pseudoephedrine early on, don’t panic. One dose doesn’t mean your baby is harmed. But do tell your provider. They can monitor for any signs of complications.
Most babies exposed to OTC meds turn out perfectly fine. The key isn’t perfection-it’s awareness. You’re already ahead by asking these questions. Now, use that knowledge to protect yourself and your baby.
Just took a Tylenol for my headache and immediately felt guilty. Thanks for this. So many of us just grab stuff without thinking.
Wow someone finally said it. I took ibuprofen at 18 weeks because I was in pain and now I'm terrified. Why is this not on every OB's website??
This is the kind of post that makes me believe in humanity again. So many of us are just winging it with OTC meds like they're candy. The fact that you broke it down like this? Pure gold. 🌟
Why are we even talking about this? Just don't take anything. That's the safest option. End of story.
The structural integrity of this article is commendable. One might argue, however, that the reliance on anecdotal evidence in the absence of longitudinal RCTs undermines its epistemological rigor. The absence of meta-analytic citations is particularly concerning.
As someone who has lived through two pregnancies across two continents, I’ve seen how cultural norms shape our approach to medication. In India, many women rely on ginger, turmeric milk, and rest - and they’re often healthier for it. In the U.S., the reflex is to reach for a pill. Neither is inherently right, but the key is awareness. We must stop treating pregnancy as a medical condition needing constant intervention and start seeing it as a natural process that deserves gentle support. The body is remarkably wise - it’s our over-reliance on pharmaceuticals that often disrupts its balance. Even Tylenol, while safer than most, isn’t neutral. The liver metabolizes it differently in pregnancy, and the placenta doesn’t filter everything. We need to normalize asking, not assuming. And we need providers who listen, not just prescribe. Let’s stop treating pregnant women like walking risk factors and start treating them like partners in their own care.
Thank you for this 🙏 Truly, this should be mandatory reading for every prenatal class. In India, we have a saying: 'Dard ka ilaj dard mein nahi, samajh mein hai' - The cure for pain isn't in more pain, but in understanding. This article embodies that. I’ve shared it with my sister-in-law who’s 6 months along. She was about to take Advil for back pain. Now she’s using a heating pad and yoga. 🌿
Of course the FDA says it's safe... until the lawsuits start. 🤡 Who really benefits from 'safe' OTC meds in pregnancy? Pharma companies. Always. I took Zyrtec because my doctor said it was fine. Then I read the fine print: 'Not tested in pregnancy beyond 12 weeks.' So... what's the real story? 😏
The pharmacokinetic shifts in pregnancy - increased volume of distribution, altered hepatic metabolism, and reduced renal clearance - necessitate a reevaluation of dosing paradigms. The current 4,000 mg acetaminophen ceiling lacks pharmacogenomic calibration. Until we integrate CYP2E1 and UGT1A1 genotyping into prenatal care, we’re operating on population averages that mask individual risk.
I used to think herbal tea was always safe until my doula told me peppermint could slow fetal growth. Now I Google every single thing. Still, this list is a lifesaver. Saved it for my next appointment. Thanks for not making me feel dumb for asking.
why do u even have to think this hard just to take a pain pill?? like just chill
Thank you for writing this. I’m 32 weeks and just realized I’ve been taking Sudafed for 3 weeks thinking it was just a cold. I’m calling my OB right now. You’re right - we don’t need to be perfect. We just need to be aware. And we’re learning. 💛
Love this! 🙌 In India, our grandmas say 'paani peelo, aaram karo' - drink water, rest. Turns out they were right. No pills needed. 🌿💧