
Buying medications shouldn’t feel like a financial gamble. If you’re taking the same pills every month-blood pressure meds, diabetes drugs, cholesterol pills-you’re probably paying more than you need to. The secret? Coordinating mail-order and local pharmacy to use each one for what they do best. It’s not complicated, but most people never try it because they don’t know how.
Why Mail-Order Isn’t Always the Cheapest Option
You’ve probably heard that mail-order pharmacies save money. And they do-sometimes. But not always. The big savings come when you get a 90-day supply of a maintenance medication instead of three separate 30-day fills. For example, a 30-day supply of generic lisinopril might cost $25 at your local pharmacy. At mail-order, a 90-day supply could be $60. That’s $15 cheaper per month, or $180 a year. Sounds good, right? But here’s the catch: if you’re on a plan that charges the same copay for 30-day and 90-day fills at your local pharmacy, you’re leaving money on the table. CVS, Walgreens, and Walmart all offer $4, $10, or $25 generic drug programs. Walmart, for instance, lets you get 90-day generic fills for $10 without insurance. That’s cheaper than most mail-order plans. You don’t need to wait for a box to arrive-you walk out with it the same day.Know Your Insurance Formulary Tiers
Your insurance doesn’t treat all drugs the same. They’re grouped into tiers: Tier 1 is usually generic, Tier 2 is preferred brand, Tier 3 is non-preferred brand, and Tier 4 is specialty. The lower the tier, the less you pay. Here’s the key: mail-order pharmacies often give you a better deal on Tier 2 and Tier 3 drugs if you order 90-day supplies. But only if your plan allows it. Check your plan’s formulary. Look up your meds on your insurer’s website or call them. Ask: “What’s my copay for a 30-day retail fill vs. a 90-day mail-order fill?” Don’t assume. One person’s $115 for 90 days might be another’s $140. Medicare Part D plans vary wildly. A 2023 Medicare Plan Finder report showed a $45 copay for a 30-day Tier 3 drug at retail, but only $115 for 90 days through mail-order. That’s a 24% daily savings. But if your local pharmacy matches that price? You skip the wait and get it now.Use Mail-Order for Maintenance Drugs Only
Not all meds belong in a mail-order box. Think of your medications in three buckets:- Maintenance drugs: Taken daily for years-like metformin, atorvastatin, levothyroxine. These are perfect for mail-order. You know the dose. You’re not changing it. You’re not waiting for side effects to settle.
- Acute or short-term drugs: Antibiotics, painkillers after surgery, steroid packs. These need to be filled fast. Mail-order takes 7-14 days. If you’re in pain or sick, you don’t have that time.
- Variable-dose drugs: Antidepressants, anticoagulants, seizure meds. These often need dose changes. If your doctor adjusts your dose, mail-order might keep sending the old version. One Reddit user lost $65 because their mail-order pharmacy sent the wrong antidepressant strength for two months.
Local Pharmacies Are More Than Just a Pickup Spot
Your local pharmacist isn’t just the person who hands you the bottle. They’re trained to catch drug interactions, spot dosage errors, and explain how to take your meds safely. A 2011 study found 78% of patients preferred face-to-face consultations with a pharmacist over phone calls from mail-order services. Also, some meds are sensitive to temperature. Insulin, biologics, and certain liquid antibiotics can lose effectiveness if they sit in a hot truck or a freezing mailbox. Local pharmacies deliver these in temperature-controlled packaging. Mail-order? Not always. The FDA warns that improper shipping can degrade meds-especially in extreme weather. If you live in a place with hot summers or cold winters, this matters. Build a relationship with one local pharmacy. Go in once a month, even if you’re not picking up anything. Ask questions. Get their number. They’ll remember your meds and help you avoid mistakes.Set Up a Refill Calendar (Seriously)
The biggest reason people give up on mail-order? They run out. You can’t just wait until you’re empty. Mail-order takes 7-14 days. If you wait until day 28, you’re out of meds for a week. Successful users set reminders 10-14 days before their supply runs out. Use your phone calendar, a paper planner, or a free app like Medisafe. One user on Reddit saved $427 a year by setting reminders for their amlodipine. They ordered 90 days at a time, paid $12.50 per fill, and never missed a dose. Pro tip: When you get a new prescription, ask your doctor to write it for 90 days with refills. That way, you can send it directly to mail-order and skip the middleman.Check If Your Local Pharmacy Matches Mail-Order Prices
Most people don’t know this: many insurance plans let you get 90-day fills at your local pharmacy for the same price as mail-order. CVS Caremark, Express Scripts, and Optum all allow this. You just have to ask. Call your pharmacy. Say: “My insurance allows 90-day fills at retail. Can you process this as a 90-day supply with my mail-order copay?” They’ll check with your plan. If they say no, call your insurer. Sometimes, the pharmacy doesn’t know the policy. You’d be surprised how often it works. GoodRx’s 2023 survey found that 68% of people who coordinated both channels saved at least $150 a year. The top 32% saved over $300. All they did was ask the right questions.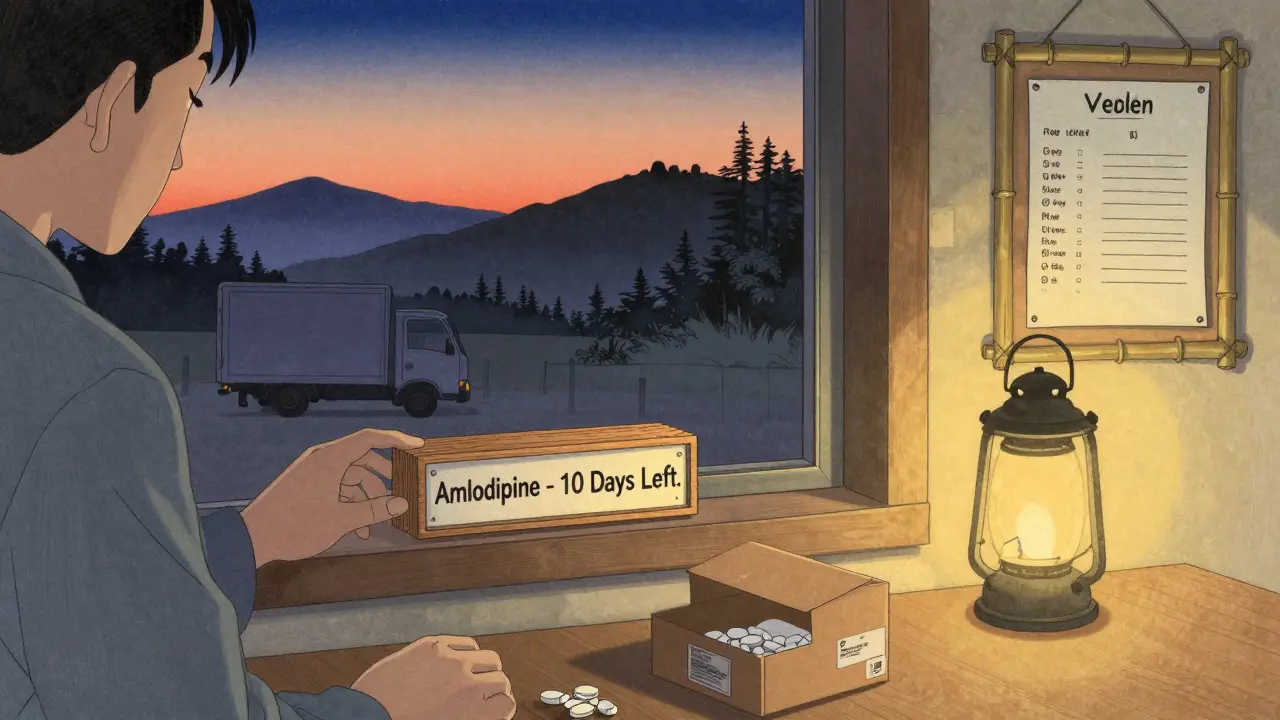
What to Do When Things Go Wrong
Even with the best plan, things break. Your mail-order pharmacy sends the wrong drug. Your insurance changes your copay without telling you. Your local pharmacy runs out of stock. Here’s how to handle it:- Monthly review: Look at your insurance statement. Compare what you paid for each med vs. what you expected. If you see a spike, call your insurer.
- Keep a list: Write down every med you take, the dose, how often, and which pharmacy you use for it. Update it every time you change something.
- Use GoodRx or Blink Health: These apps show cash prices. Sometimes, paying cash at a local pharmacy is cheaper than your insurance copay.
- Ask for a 30-day emergency fill: If your mail-order is delayed, your local pharmacy can usually give you a 30-day supply at your usual copay. Just call ahead.
The Future Is Integrated
By 2025, most insurance plans will let you switch between mail-order and local pharmacies with one click. UnitedHealthcare’s Optum Perks and Express Scripts’ Pharmacy Choice program already do this. Your refill schedule syncs across both. No more double orders or missed fills. Medicare’s 2024 Part D changes will also standardize 90-day pricing across channels. That means the old advantage of mail-order might shrink. But the strategy won’t disappear-it’ll just get smarter. The goal isn’t to pick one pharmacy. It’s to use both wisely.Start Today: Your 5-Step Plan
1. List every medication you take. Mark which are maintenance, acute, or variable-dose. 2. Call your insurer and ask for the exact copay for each med at retail vs. mail-order for 30-day and 90-day supplies. 3. Visit your local pharmacy and ask if they can fill 90-day supplies at your mail-order price. Don’t take no for an answer. 4. Set calendar reminders 10-14 days before each maintenance med runs out. 5. Review every 3 months. Insurance plans change. So should your plan. You don’t need to be a pharmacist to save hundreds a year. You just need to know where to look-and when to ask.Can I use mail-order for all my medications?
No. Mail-order works best for maintenance medications you take daily for months or years, like blood pressure or diabetes drugs. Avoid using it for antibiotics, new prescriptions, or meds that require dose changes. These need to be filled quickly and monitored by a pharmacist, which local pharmacies do better.
Is mail-order always cheaper than local pharmacies?
Not always. Many local pharmacies, like Walmart and CVS, offer 90-day generic fills for $10 or $15 without insurance-sometimes cheaper than mail-order. Always compare prices using your insurance details. Some plans even let you get 90-day fills at your local pharmacy at the same price as mail-order.
How long does mail-order take to arrive?
Typically 7-14 business days. This makes it unsuitable for urgent needs. If you’re starting a new medication or need something right away, use your local pharmacy. Always order your maintenance meds at least 10 days before you run out to avoid gaps in treatment.
Can I save money if I don’t have insurance?
Yes. Cash prices at local pharmacies like Walmart, Costco, or through apps like GoodRx and Blink Health are often lower than insurance copays. For example, a 90-day supply of generic lisinopril can cost $10 at Walmart. Use these tools even if you’re insured-sometimes paying cash is cheaper.
What if my mail-order pharmacy sends me the wrong medication?
Call the pharmacy immediately and report the error. Keep the medication and packaging. Then contact your doctor and local pharmacist to confirm the correct dose. If you took the wrong drug, seek medical advice. To prevent this, always verify your prescription details when you order and ask your doctor to send electronic prescriptions directly to your pharmacy.
This is actually one of the most practical guides I’ve seen on medication savings. I’ve been using this exact strategy for my dad’s statins and metformin-90-day mail-order for those, local pharmacy for anything new or as-needed. Saved us $280 last year alone. Also, never underestimate the pharmacist’s advice-they caught a potential interaction I missed on GoodRx.
LMAO this is so basic it’s almost insulting 😂 You think people don’t know Walmart does $10 generics? My grandma’s been doing this since 2012. Also, mail-order? More like mail-delay. My insulin sat in a Texas mailbox for 10 days in July. FDA warning? Bro, it’s 2025.
bro why are you overthinking this. just go to walmart. $10 for everything. done. why you need all these tiers and formularies and calendars?? i just pay cash and move on. also mail order = slow. my cat died waiting for his meds once. not a joke.
Just wanted to say this is the kind of post that makes me feel less alone in this mess. I’ve been doing the 90-day mail-order for my blood pressure med but keeping my anxiety script local. Never thought to ask if my pharmacy could match the mail-order price. gonna call tomorrow. thanks for the nudge
There is a philosophical dimension to this: the commodification of health. We are conditioned to optimize cost, efficiency, and convenience-yet the human element-the pharmacist’s gaze, the tactile exchange of the bottle, the quiet reassurance-cannot be algorithmically replicated. The system rewards automation. But the body remembers intimacy. Perhaps the real savings is not in dollars, but in dignity.
so i tried this last month and it actually worked. i set a reminder for my levothyroxine and got the 90-day at walmart for $10. i felt like a genius. also my pharmacist gave me a free lollipop. small wins. keep sharing stuff like this
Thank you for this thoughtful, well-researched piece. I especially appreciate the emphasis on temperature-sensitive medications-many forget that insulin and biologics are not just pills. I’ve worked in community pharmacy for 18 years, and I’ve seen too many patients suffer from delayed or degraded meds because they trusted mail-order without verifying shipping conditions. Always ask your pharmacist: ‘Is this safe to ship?’ It’s a simple question with life-altering answers. Also, setting refill reminders is one of the most powerful habits a chronic illness patient can adopt. Well done.
As a former claims analyst for a major PBM, I can confirm: 90-day retail fills at mail-order pricing are not only possible-they’re often overlooked. The system is designed to route patients to mail-order, but the contracts allow retail substitution. Most pharmacies don’t initiate the conversation. You have to. Use the phrase: ‘I’m requesting a 90-day retail fill under my plan’s mail-order benefit.’ It triggers the right protocol. We saved members $1.2M last year just by coaching them to ask.
Y’all are overcomplicating this. America has the best healthcare system in the world. If you can’t save $150 a year on meds, you’re not trying. Walmart. GoodRx. Cash. Done. Stop whining about formularies. Get off your phone and go to the pharmacy. #MakeAmericaHealthyAgain