When your kidneys aren’t working well, what you eat matters more than you might think. Especially protein. Too much can overload your kidneys. Too little can leave you weak, hungry, and losing muscle. Finding the right balance isn’t about cutting protein completely-it’s about getting the right amount at the right time, based on how far your kidney disease has progressed.
What Protein Does to Your Kidneys
Your kidneys filter waste from your blood. When you eat protein, your body breaks it down into nitrogen waste, mostly urea. Healthy kidneys handle this easily. But when they’re damaged, that waste builds up. That’s why doctors have long recommended lowering protein intake in chronic kidney disease (CKD). It’s not magic-it’s physics. Less protein means less waste. Less waste means less strain. Studies show this can slow the decline of kidney function and delay the need for dialysis by 6 to 12 months.But here’s the twist: not all protein is the same. And not all people with CKD need the same amount. Age, muscle mass, diabetes, and even how well you’re eating overall change the equation. A 70-year-old with stage 3 CKD and low appetite needs different advice than a 45-year-old with stage 2 CKD who’s active and eats well.
Protein Targets by CKD Stage
The Kidney Disease Outcomes Quality Initiative (KDOQI) and other major groups have laid out clear targets based on your kidney function, measured by GFR (glomerular filtration rate).- CKD Stage 1-2 (GFR ≥60): Stick to 0.8 grams of protein per kilogram of ideal body weight per day. For a 150-pound person (68 kg), that’s about 54 grams. This isn’t a low-protein diet-it’s just avoiding excess. Most people eat more than this anyway. The goal here is prevention, not restriction.
- CKD Stage 3 (GFR 30-59): Drop to 0.55-0.60 grams per kg. For that same 150-pound person, that’s 40-54 grams daily. This is where many start to feel the pinch. Hunger sets in. Muscle feels softer. That’s why quality matters more than ever.
- CKD Stage 4 (GFR 15-29): Stay at 0.6 grams per kg. Some experts suggest going as low as 0.55 if GFR drops below 25. At this stage, protein-energy wasting is a real risk. About 30-50% of people in this group become malnourished if not carefully managed.
- CKD Stage 5 (GFR <15, not on dialysis): Same range: 0.55-0.60 g/kg. But if you’re already on dialysis, your protein needs jump back up-sometimes to 1.0-1.2 g/kg. Dialysis removes protein, so you need to replace it.
Diabetics with CKD need special care. The American Diabetes Association recommends 0.8-0.9 g/kg to protect kidneys without risking low blood sugar or muscle loss. Don’t assume the same rule applies to everyone.
Plant vs. Animal Protein: The Real Difference
Not all protein sources are created equal when it comes to kidney health. Animal proteins-like beef, chicken, eggs, and dairy-produce more urea and phosphate per gram than plant proteins. They also generate more advanced glycation end products (AGEs), which cause inflammation and oxidative stress in damaged kidneys.Plant proteins-beans, lentils, tofu, nuts, and whole grains-produce 20-30% less waste. A 2021 study found that swapping just 30% of animal protein for plant protein cut the risk of CKD worsening by 14% and lowered death risk by 11%. That’s huge.
But here’s the catch: plant proteins are often low in essential amino acids like lysine and methionine. Your body can’t make those. You need them to maintain muscle and repair tissue. So if you’re eating mostly plants, you have to plan smarter. Combine soy (a complete plant protein) with grains and legumes. A bowl of lentil soup with brown rice? That’s a smart combo.
On the flip side, animal proteins are complete. One egg, one chicken breast, one serving of fish-each gives you all the amino acids you need. That’s why guidelines say at least half your protein should come from high-quality sources if you’re in stage 4 or 5. Eggs, milk, fish, and lean poultry are your best bets.

Why Many People Struggle
It’s not just about numbers. It’s about life.A 2024 survey by the American Kidney Fund found that 74% of people on low-protein diets felt constantly hungry. 62% said they felt weak. 58% avoided eating with family because their meals looked so different. One Reddit user wrote: “Cutting my protein from 100g to 45g made me feel like I was starving every day.”
That’s why so many people quit. Only about 58% stick to low-protein diets long-term, according to the Cochrane Review. But here’s the good news: those who work with a renal dietitian? 82% say they feel better and stick with it.
Why? Because dietitians don’t just give numbers. They give meals. They teach you how to use apps like MyFitnessPal with renal databases. They help you meal prep kidney-friendly recipes from trusted sources like Kidney Kitchen, which gets over a million visits a month. They show you how to track protein in mixed dishes-something 87% of patients struggle with.
Tools That Actually Help
You don’t have to guess. There are tools built for this.- Protein calculators: The National Kidney Foundation’s free app lets you enter your weight, stage, and goals. It tells you exactly how many grams you can have each day.
- Renal-specific food databases: Apps like MyFitnessPal now have filters for low-potassium, low-phosphorus, low-protein foods. Use them.
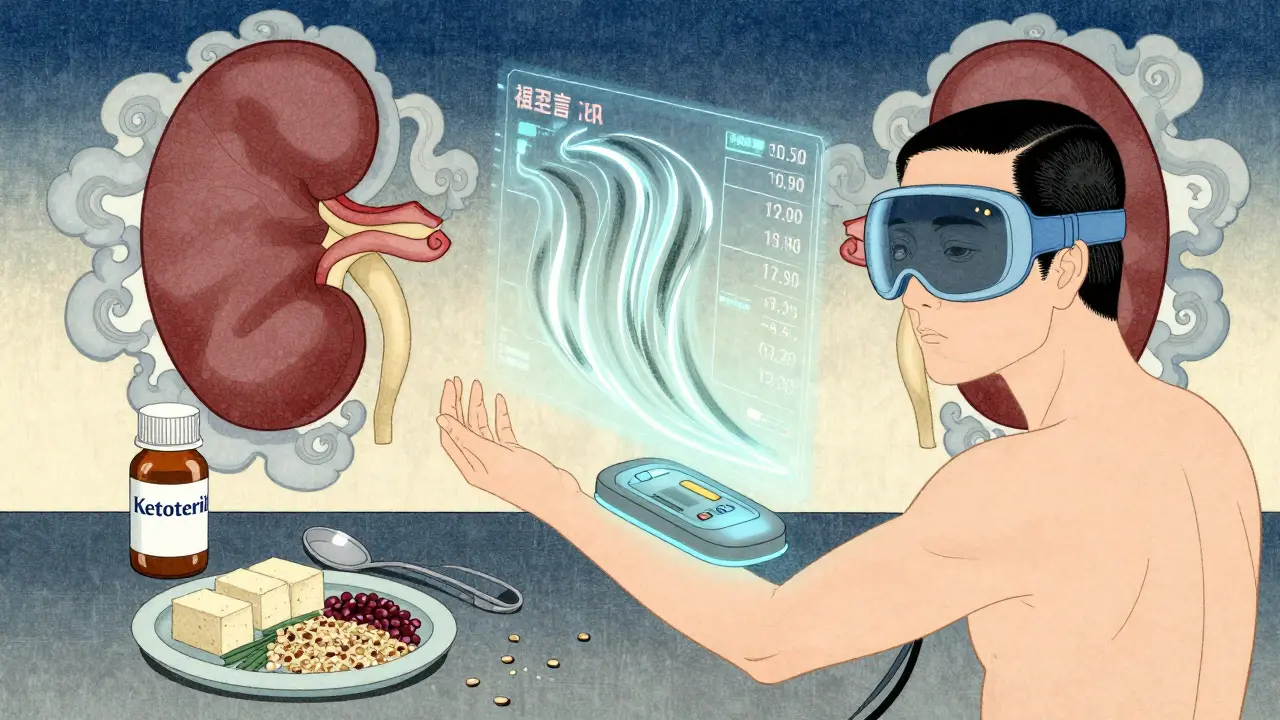
- Keto acid analogues: These are prescription supplements (like Ketosteril) that provide essential amino acids without the nitrogen waste. Used by 15% of stage 4-5 patients in Europe, they help you eat less protein without losing muscle.
- Meal prepping: Cook a big batch of egg-white omelets, grilled chicken breast, and quinoa. Portion them out. Freeze. You’ll eat better and waste less time.
Structured education programs increase adherence by over 3 times. That’s not a small thing. It’s life-changing.
The Bigger Picture: It’s Not Just About Quantity
There’s a growing debate in nephrology. Some experts, like Dr. Kamyar Kalantar-Zadeh, argue that for older adults with CKD, higher protein intake may actually save lives. Why? Because many die from heart disease before their kidneys fail. Starving them of protein might weaken them more than help.That’s why the National Kidney Foundation’s 2023 guidelines say: individualize. If you’re 80, frail, and losing weight, 0.6 g/kg might be too low. If you’re 50, active, and overweight, you might be fine at 0.8 g/kg.
Future tools are even smarter. The NIH-funded PRECISE-CKD trial is testing whether protein needs should be based on your body’s actual urea production-not just your weight. Imagine a wearable that tracks your protein metabolism in real time. That’s coming.
And the market is responding. The global renal nutrition market hit $1.7 billion in 2023. Companies are developing plant-based protein powders with reduced potassium. Insurance now covers up to 5 hours of dietitian visits per year for Medicare patients with CKD. That’s progress.
What to Do Next
If you or someone you care about has CKD:- Find out your exact GFR and CKD stage. Ask your nephrologist.
- Calculate your protein target using your weight and stage. Use the NKF app.
- Focus on high-quality protein sources-eggs, fish, lean meat, soy.
- Include more plant proteins, but pair them wisely (rice + beans, hummus + whole wheat pita).
- Work with a renal dietitian. Even one session can change everything.
- Track your hunger, energy, and muscle strength. If you’re getting weaker, your protein might be too low.
Renal nutrition isn’t about perfection. It’s about smart, sustainable choices. You don’t need to eat like a monk. You just need to eat like someone who’s protecting their kidneys-for as long as possible.
How much protein should I eat if I have stage 3 CKD?
For stage 3 CKD, aim for 0.55 to 0.60 grams of protein per kilogram of your ideal body weight per day. For example, if you weigh 150 pounds (68 kg), that’s about 40 to 54 grams of protein daily. Focus on high-quality sources like eggs, fish, chicken, and soy. Avoid excessive intake-more than 0.8 g/kg can speed up kidney damage. But don’t go too low-you still need protein to maintain muscle and prevent weakness.
Can I get enough protein on a plant-based diet with CKD?
Yes, but it takes planning. Plant proteins like beans, lentils, and tofu are lower in waste products, which is good for your kidneys. But they’re often missing key amino acids like lysine and methionine. To get a complete profile, combine different sources-like rice and beans, or hummus with whole grain bread. Soy is one of the few complete plant proteins. You may also need to include small amounts of animal protein (like eggs or dairy) to meet your needs without overloading your kidneys.
Why do I feel so tired on a low-protein kidney diet?
Low protein intake can lead to muscle loss and protein-energy wasting, especially in stages 3-5. Feeling weak, hungry, or tired is common if you’re not getting enough high-quality protein or enough total calories. Many people cut protein but forget to replace the calories with carbs and healthy fats. Talk to a renal dietitian-they can help you adjust your plan so you get enough energy without harming your kidneys.
Do I need to avoid all red meat with CKD?
You don’t need to avoid it completely, but you should limit it. Red meat produces more waste and inflammation than other protein sources. It also contains more phosphorus and advanced glycation end products (AGEs), which can worsen kidney damage. If you eat red meat, keep portions small-about the size of a deck of cards-and choose lean cuts. Better options include fish, chicken, eggs, and plant proteins. Even one or two small servings a week is fine if your overall protein is controlled.
Should I use protein supplements for CKD?
Regular protein powders (whey, casein, soy isolate) are usually not recommended-they add too much nitrogen waste. But there’s a special type called keto acid analogues (like Ketosteril), which provide essential amino acids without the waste. These are prescription-only and used mainly in stage 4-5 CKD to help you eat less protein without losing muscle. Always talk to your doctor before using any supplement. Over-the-counter protein powders can hurt your kidneys if you’re not on dialysis.
How do I track protein in mixed dishes like pasta or stir-fry?
Use apps like MyFitnessPal with a renal-specific food database, or the NKF’s Protein Target Calculator. For mixed dishes, estimate the protein from each ingredient: 1 cup cooked pasta = 8g, 3 oz chicken = 21g, 1/2 cup beans = 7g. Add them up. Many renal dietitians provide portion guides and sample meal plans. Meal prepping in advance helps-you know exactly what’s in each container. Don’t guess. Measure.
Is it safe to eat more protein if I’m older with CKD?
For older adults (65+), higher protein intake (up to 0.8-1.0 g/kg) may be safer than strict restriction. Many die from heart disease before reaching dialysis, and muscle loss increases fall risk and hospital stays. A 2024 JAMA study found older CKD patients on higher protein diets lived longer. But this depends on your overall health. If you’re frail or losing weight, talk to your doctor. If you’re active and eating well, you might not need to cut as much. Individualization is key.
Okay but let’s be real-this whole ‘low protein for CKD’ thing is just Big Nephro pushing a diet that makes people weak so they’ll need more meds and dialysis. My uncle in Ontario ate steak three times a week at stage 4 and lived to 82. Kidneys aren’t fragile glass figurines. They’re organs, not tea cups. Stop infantilizing patients.
❤️ I just want to say thank you for writing this with so much care. I’m a stage 3 CKD mom of three and I’ve been terrified of messing up my diet. This gave me clarity-and hope. I’m going to see a renal dietitian next week. You’re not alone out there. We’ve got this 💪
While the general recommendations presented are consistent with current KDOQI guidelines, one must consider the heterogeneity of metabolic responses among individuals with chronic kidney disease. The assumption that protein intake can be universally calibrated via body weight alone may overlook critical variables such as lean body mass, inflammatory markers, and residual renal function. Further longitudinal data are warranted.
Yeah, I’ve been doing the 0.6g/kg thing for a year. Honestly? I feel okay. Not amazing, not terrible. Just… okay. I eat eggs and tofu mostly. Don’t stress too much. Just keep track. And if you’re hungry, eat more rice. It’s not gonna kill you.
so like… i tried to use myfitnesspal but i kept gettin confused with the renal filter? like… is quinoa low protein or no?? and why does it say 1 cup = 8g but my bowl looks like 3 cups?? someone pls help
Consistency beats perfection. Start with one meal a day that’s kidney-smart. Maybe swap your morning bacon for egg whites. Then add one plant-based dinner. Small wins build momentum. You don’t need to overhaul your life overnight. Just show up.
Let’s deconstruct the dogma, shall we? The protein restriction paradigm is a relic of the 20th century’s reductionist biochemistry-a Cartesian fantasy where the kidney is merely a sieve, and protein is just urea’s taxi. But we now know that amino acids modulate mTOR, fibroblast growth factor 23, and even gut microbiome dysbiosis. To reduce protein without addressing systemic inflammation is like turning off the alarm while the house burns. The real enemy isn’t protein-it’s metabolic inertia. We must transition from quantity-based prescribing to quality-based biofeedback. Enter: wearable urea flux monitors. The future is not low-protein. It’s *precision-protein*.
Thank you for providing such a comprehensive and clinically grounded overview. The integration of evidence-based targets with practical dietary strategies enhances patient adherence and outcomes significantly. This resource will be invaluable for both clinicians and patients navigating the complexities of renal nutrition.
Wait-so if I’m 70, frail, and have stage 3 CKD… and I’m losing muscle… and I’m scared of eating meat… should I really be eating only 40g of protein? That’s less than one chicken breast. I feel like I’m being told to starve myself to survive. This doesn’t make sense. I’m not a lab rat.
I was in stage 4 and felt like a ghost until I started eating more eggs and soy. I used to think ‘plant protein’ meant sad salads. Turns out, lentil curry with brown rice and a sprinkle of cheese? Life-changing. You don’t have to eat like a monk. Just eat smarter. And if you’re tired-your body’s telling you something. Listen.
OMG YES. I’ve been eating plant-based for 3 years with CKD and I was SO worried I’d lose muscle. But I started combining soy + rice + nuts every day and now I’m stronger than ever. I even started hiking! You CAN do this. It’s not about deprivation-it’s about smart swaps. You’re not broken. You’re adapting.
My dad’s on dialysis now and they told him to eat 1.1g/kg. He was confused because the article said to cut protein. So I’m confused too. Why does dialysis change everything? Someone explain this without the jargon?
Just wanted to say-your post helped me finally talk to my doctor about keto acid analogues. I didn’t even know they existed. We’re scheduling a consult with a renal dietitian next week. You’re not just sharing info-you’re changing lives. Thank you.