
When a shingles rash finally fades, many expect relief. Instead, a lingering, burning ache can take over - that’s Postherpetic Neuralgia, a form of chronic neuropathic pain that follows Herpes Zoster. Pinpointing PHN early is tricky because the symptoms overlap with other pain conditions, and the tools doctors have aren’t always precise. This guide walks through the biggest hurdles, the tests that help, and practical tips to make the diagnostic journey less confusing.
Why Diagnosis Feels Like Guesswork
Imagine trying to identify a single instrument in an orchestra after the music stops. The notes linger, but the source isn’t obvious. PHN works the same way: the nerve damage caused by the varicella‑zoster virus (VZV) leaves a patchwork of sensations - burning, stabbing, throbbing - that can mimic arthritis, migraine, or even mental‑health‑related somatic pain.
- Symptoms often appear weeks after the rash clears, making the timeline fuzzy.
- No single lab test confirms PHN; clinicians rely on patterns and exclusion.
- Older adults, who are most at risk, may have other age‑related pain sources complicating the picture.
These factors create a diagnostic gray zone where both patients and doctors wonder: "Is this still shingles, or something else?"
Key Entities in the Diagnostic Puzzle
Before diving into tools, it helps to know the main players:
- Herpes Zoster: The acute shingles infection that triggers nerve inflammation.
- Varicella Zoster Virus (VZV): The virus that reactivates from dormant state in sensory ganglia.
- Neuropathic Pain: Pain arising from damaged nerves, characterized by burning, tingling, or electric‑shock sensations.
- Chronic Pain: Pain persisting longer than three months, often affecting quality of life.
- Quality of Life: A broad measure that includes physical comfort, sleep, mood, and daily functioning.
Clinical Assessment - The First Line
Doctors start with a detailed history and physical exam. The goal is to link the current pain to a recent shingles episode.
- Ask when the rash appeared, its location, and how long it lasted.
- Map the pain’s distribution - PHN usually follows the dermatome where the rash was.
- Evaluate pain quality (burning vs aching) and triggers (cold, wind, pressure).
- Screen for comorbidities like diabetes or depression that could amplify pain.
If the narrative fits and the pain persists beyond three months, clinicians often label it PHN - but the label is still provisional.
Objective Tests - Adding Some Science
Because the history can be vague, objective measures help corroborate nerve involvement.
| Tool | What it Measures | Pros | Cons |
|---|---|---|---|
| Clinical Assessment | Patient‑reported symptoms + dermatomal pattern | Quick, low cost | Subjective, relies on memory |
| Quantitative Sensory Testing (QST) | Thermal and mechanical thresholds | Detects subtle sensory loss | Requires specialized equipment, time‑consuming |
| Nerve Conduction Study (NCS) | Electrical conduction speed in peripheral nerves | Objective, quantifiable | May miss small‑fiber involvement, invasive needles |
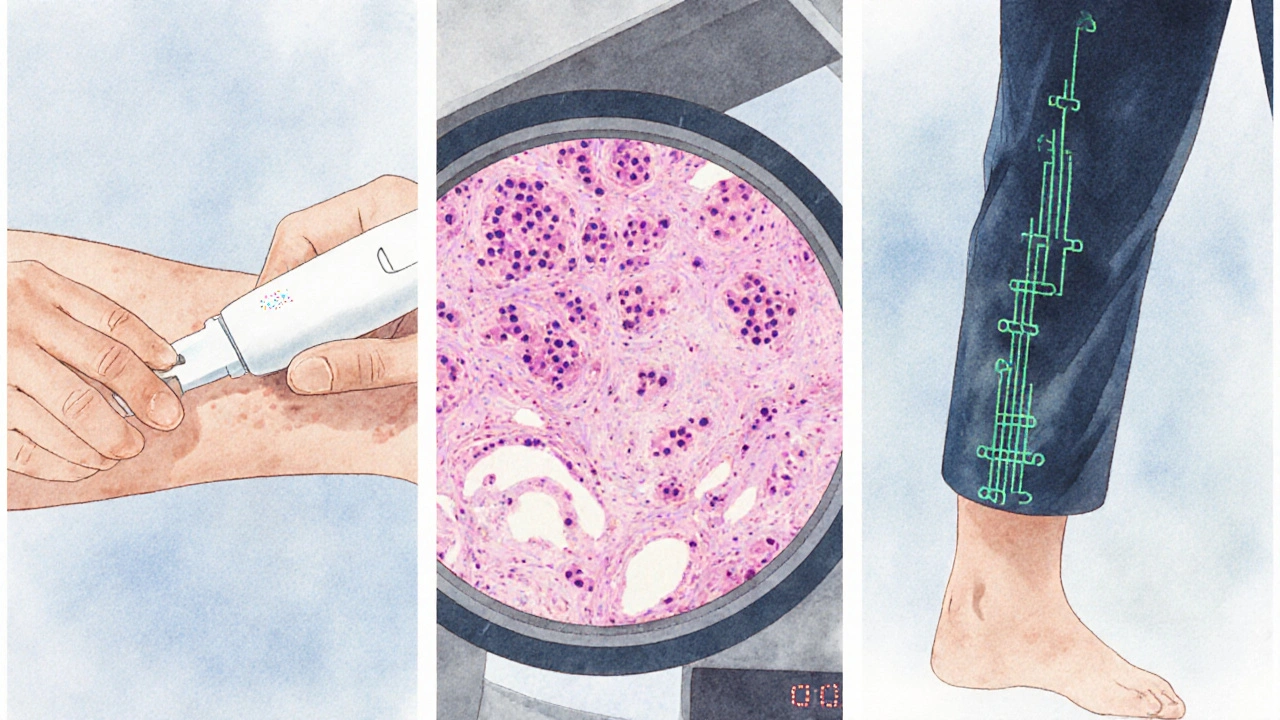
| Skin Biopsy (intra‑epidermal nerve fiber density) | Density of small nerve fibers | Gold standard for small‑fiber neuropathy | Invasive, requires pathology expertise |
In practice, clinicians rarely run all four tests. Most rely on QST if the pain pattern is ambiguous, and they may order a skin biopsy when small‑fiber loss is suspected but not proven.
When Tests Disagree - Navigating Conflicts
It’s not unusual for QST to show abnormal thresholds while nerve conduction appears normal. Small fibers carry pain signals, but standard NCS focuses on large‑myelinated fibers. In such cases, the skin biopsy becomes decisive because it directly visualizes small‑fiber density.
Another challenge is distinguishing PHN from other post‑viral neuropathies (e.g., COVID‑related neuralgia). A thorough medication review helps; some analgesics like Gabapentin can mask pain intensity, leading to under‑reporting.
Impact on Treatment Decisions
Accurate diagnosis isn’t just academic - it directs therapy. Early antiviral therapy (Antiviral Therapy such as acyclovir) can reduce PHN risk if started within 72hours of rash onset. Once PHN is confirmed, first‑line agents include gabapentinoids, tricyclic antidepressants, or topical agents like Capsaicin Patch. Each choice hinges on the patient’s comorbidities, pain intensity, and whether tests suggest small‑fiber loss.
For example, a patient with reduced intra‑epidermal nerve fiber density may respond better to topical capsacin, which desensitizes remaining fibers, whereas someone with predominant allodynia might need gabapentin to dampen central sensitization.

Practical Tips for Patients and Clinicians
- Document the rash timeline. Even a photo of the original shingles can be a useful reference.
- Ask about triggers - cold air or tight clothing often worsens PHN.
- If pain persists beyond a month, request a QST or skin biopsy referral; early objective data can shorten the trial‑and‑error period of medication.
- Keep a pain diary that records intensity (0‑10 scale), quality, and activities. This data helps clinicians see patterns that may point to PHN.
- Don’t ignore mood changes. Depression and anxiety can amplify pain perception, so screening tools like PHQ‑9 add valuable context.
Key Takeaways
- Postherpetic Neuralgia often hides behind vague, lingering pain that mimics other conditions.
- Clinical history is essential, but objective tests such as QST, nerve conduction studies, and skin biopsies improve diagnostic confidence.
- Small‑fiber neuropathy is the hallmark of PHN; skin biopsy remains the gold standard when other tests are inconclusive.
- Accurate diagnosis guides targeted therapies, from antivirals early on to gabapentin, tricyclics, or capsaicin patches later.
- Patients who track symptoms and request appropriate testing can shorten the time to effective pain relief.
Frequently Asked Questions
How long after a shingles rash can PHN develop?
Pain can start while the rash is still present, but most clinicians define PHN when pain persists at least three months after the rash has healed. Some patients notice lingering discomfort earlier, which signals a higher risk of chronic pain.
Can a blood test confirm PHN?
No. There’s no blood marker that definitively diagnoses PHN. Diagnosis relies on clinical patterns and, when needed, specialized tests that assess nerve function or structure.
Is a skin biopsy painful?
A skin biopsy uses a small punch tool (3‑4mm). Local anesthetic numbs the area, so most patients feel only mild pressure. The procedure takes a few minutes and heals within a week.
What role does early antiviral treatment play?
Starting antivirals (acyclovir, valacyclovir, or famciclovir) within 72hours of rash onset can shorten the infection and lower the chance of nerve damage, reducing PHN incidence by up to 50% in some studies.
When should I ask my doctor for a referral to a pain specialist?
If pain remains high (≥7/10) after four weeks of guideline‑based medication, or if it interferes with sleep, work, or mood, a specialist can offer advanced options like nerve blocks, neuromodulation, or tailored physiotherapy.
Wow, this guide really breaks down the PHN puzzle in a way that even my grandma could follow 😊. The analogies with the orchestra are spot‑on, and the tip about photographing the rash is genius. Thanks for making a complex topic feel like a chat over coffee!
While the content is solid, I can’t help noticing several missing commas that change the meaning of sentences. For instance, "When pain persists beyond a month, request a QST" could be clearer with a pause. Precision matters, especially in medical writing.
Absolutely! I love how the article encourages patients to keep a pain diary – that’s a game‑changer for tracking patterns and communicating with clinicians. By documenting triggers like cold wind or tight clothing, you give doctors concrete data rather than vague complaints. It also empowers patients, turning them from passive recipients into active partners in their care. And remember, a diary isn’t just numbers; adding notes about mood swings can reveal the hidden link between anxiety and pain intensity. Keep spreading this positive, hopeful message!
The discussion of quantitative sensory testing (QST) really hits the sweet spot of clinical‑neurophysiology jargon. Using terms like thermal thresholds and mechanical allodynia helps bridge the gap between primary care and pain specialists. Plus, the nod to small‑fiber neuropathy emphasizes why we need more than just conventional nerve conduction studies. It’s a solid call‑to‑action for multidisciplinary teams.
This post is overly optimistic and ignores the reality that many patients never get access to QST or skin biopsies due to cost and insurance barriers
Indeed, the financial hurdle, especially for uninsured patients, is a major barrier, and without proper reimbursement, clinicians may hesitate to order costly tests, such as skin biopsies, which, although considered the gold standard, can be prohibitive for many, leading to underdiagnosis, and ultimately, suboptimal management of PHN, a situation that calls for systemic reform, and better insurance coverage policies.
Honestly this article is spot on, but i think they could have added more about how PHN can ruin your life in the long run, like i have a cousin who suffers and it's heartbreaking.
Appreciating the balanced perspective here – the guide acknowledges both clinical challenges and practical patient steps without sounding preachy. It’s a good reference for anyone navigating post‑shingles pain.
While the tone is appreciated, it’s odd to see a medical article gloss over the ethical considerations of invasive skin biopsies – patients deserve clearer consent information.
Oh great, another “expert” telling us to trust the system while the pharma giants sit on a mountain of data about nerve‑pain meds that they don’t want us to see. The whole narrative feels like a carefully curated PR piece, pushing gabapentinoids as the default without mentioning the real‑world addiction concerns. Sure, early antivirals help, but why is there no critique of the profit‑driven push for brand‑name drugs? And the mention of capsacin patches? Probably just another way to keep the pipeline bubbling. Honestly, it’s hard to trust a guide that whispers about “practical tips” while ignoring the big picture of medical‑industry collusion. Remember, every recommended test or drug comes with a price tag, both financially and in terms of side‑effects, and the article barely scratches the surface.
The key takeaway is to track symptoms diligently.
In terms of diagnostic rigor, it is imperative to emphasize that the absence of a definitive laboratory biomarker necessitates a reliance on comprehensive clinical evaluation. The temporal correlation between the dermatome of the original rash and the persistent neuropathic descriptors remains the cornerstone of diagnosis. Additionally, the utilization of quantitative sensory testing provides an objective assessment of sensory thresholds, thereby augmenting the clinical impression. When discrepancies arise between QST findings and nerve conduction studies, a skin biopsy for intra‑epidermal nerve fiber density should be considered, given its status as the gold standard for small‑fiber neuropathy. Early initiation of antiviral therapy within the 72‑hour window demonstrably reduces the incidence of post‑herpetic sequelae. Consequently, a multidisciplinary approach, integrating pain specialists, dermatologists, and primary care providers, optimizes patient outcomes.
Great job laying out the steps so clearly! I especially appreciate the reminder to screen for depression – mental health truly affects pain perception. Let’s keep encouraging patients to stay proactive with diaries and open communication.
One must acknowledge that true compassion in medicine goes beyond diagnostics; it requires a moral commitment to universal access, lest we perpetuate inequities under the veneer of clinical excellence. Our duty is to champion equitable care, not merely to fine‑tune protocols while the marginalized suffer.
Reading this comprehensive guide reminds me of the first time I encountered a patient with stubborn post‑herpetic neuralgia. The patient, a 68‑year‑old retired teacher, came in complaining of a relentless burning sensation that lingered weeks after a seemingly ordinary shingles rash cleared. She described the pain as “like tiny fireworks exploding under my skin,” a vivid metaphor that instantly highlighted the neuropathic nature of her suffering. After a meticulous review of her medical history, I noted an otherwise unremarkable profile, except for mild hypertension managed with a low‑dose ACE inhibitor. The physical exam revealed hyperesthesia confined to the T5 dermatome, matching the original rash distribution, which was a crucial diagnostic clue. I explained to her that PHN often masquerades as other chronic pains, and that early antiviral therapy is the most effective preventive strategy, though in her case the window had closed. We decided to proceed with quantitative sensory testing to quantify her thermal and mechanical thresholds, as the literature suggests this can guide therapeutic choices. The QST results were striking: a significant reduction in cold detection thresholds, confirming small‑fiber involvement. Given these findings, I recommended a skin biopsy to assess intra‑epidermal nerve fiber density, the gold standard for confirming small‑fiber neuropathy. The biopsy, performed under local anesthesia, showed a marked reduction in nerve fiber density, corroborating our clinical suspicion. Armed with this objective data, we initiated a tailored treatment plan: low‑dose gabapentin, a topical capsaicin patch applied for 60 minutes twice weekly, and a brief course of amitriptyline to address sleep disturbances. I also emphasized the importance of a pain diary, encouraging her to log intensity, triggers, and mood fluctuations, which later proved invaluable for medication titration. Over the next six weeks, her pain scores gradually declined from an 8/10 to a manageable 3/10, and she reported improved sleep quality and a renewed sense of hope. This case illustrates the critical role of integrating clinical acumen with objective testing, patient education, and a multidisciplinary approach to conquer the challenges of PHN. Moreover, it underscores how a compassionate, evidence‑based strategy can transform a patient’s quality of life, turning despair into resilience.
Oh, wonderful, another heroic tale of a doctor playing detective while the pharmaceutical industry watches profit margins rise. The relentless push for gabapentin and capsaicin patches feels less like patient‑centered care and more like a marketing showcase. And sure, a pain diary is helpful, but why not mention the hidden costs of these “tailored” regimens? The narrative glosses over systemic barriers and pretends that every patient can simply follow the protocol.