Polydipsia Symptom Checker
Check Your Symptoms
This tool helps you assess whether your thirst might indicate a medical condition versus simple dehydration. Answer the questions below to get personalized guidance.
Enter your symptoms to see assessment results.
Important Note: This tool is for informational purposes only and does not replace professional medical advice. Always consult your healthcare provider for proper diagnosis and treatment.
Increased thirst (polydipsia) is a physiological response that compels a person to drink more fluids than usual. It can arise from simple dehydration, but it also serves as a red flag for underlying medical conditions. Recognizing the patterns behind excess thirst helps you and your clinician separate a harmless water‑craving from a sign that needs further testing.
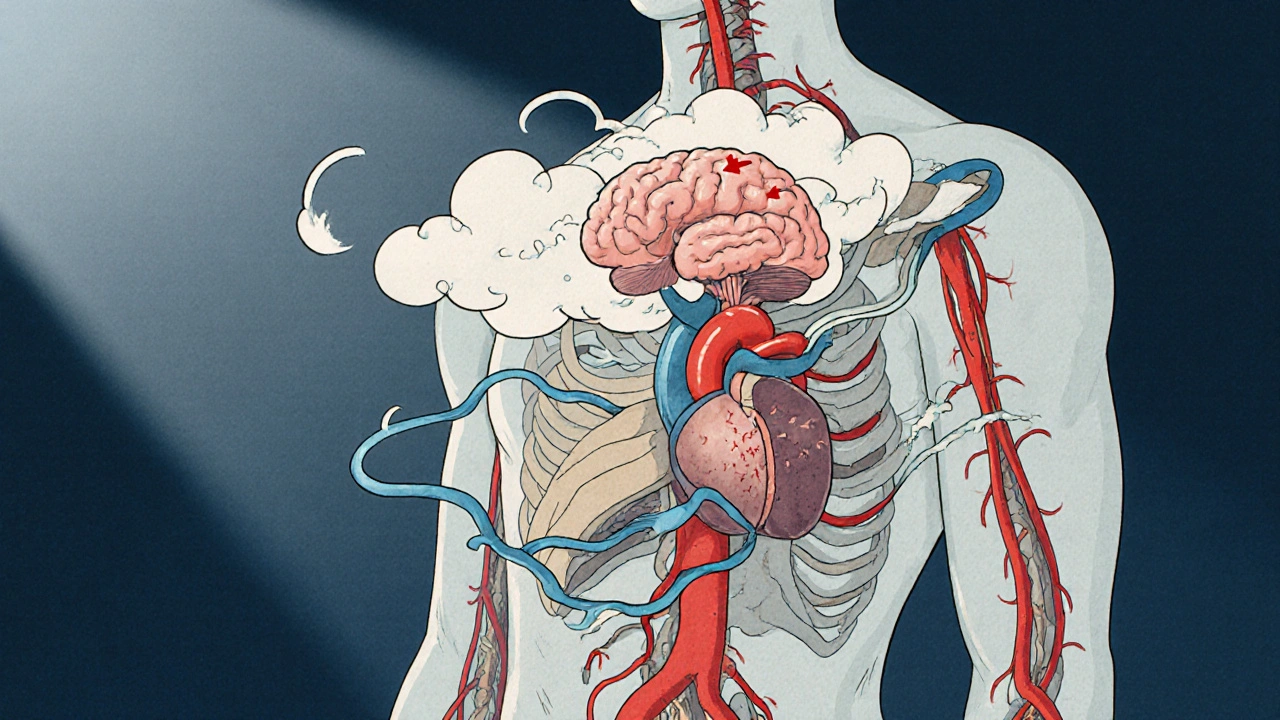
How the Body Controls Thirst
Two key sensors keep tabs on water balance: the osmoreceptors in the hypothalamus and the stretch receptors in the heart and blood vessels. When blood‑sugar rises, when sodium climbs, or when blood volume drops, these receptors trigger the feeling of thirst.
Understanding which sensor is firing gives clues about the root cause. For example, high blood‑sugar primarily activates osmoreceptors, while low blood volume stimulates stretch receptors.
Medical Conditions That Show Up as Increased Thirst
Below is a quick look at the most common health issues that turn up on a doctor’s radar when a patient reports persistent thirst.
| Condition | Why Thirst Occurs | Typical Lab Findings | First‑line Treatment |
|---|---|---|---|
| Diabetes mellitus | Elevated glucose raises plasma osmolality. | Fasting glucose >126 mg/dL, HbA1c ≥6.5%. | Lifestyle changes + oral hypoglycemics or insulin. |
| Diabetes insipidus | Deficiency of antidiuretic hormone (ADH) or renal resistance. | Serum sodium normal‑high, dilute urine (<300 mOsm/kg). | Desmopressin for central DI; thiazides for nephrogenic. |
| Hypercalcemia | Calcium interferes with renal concentrating ability. | Serum calcium >10.5 mg/dL, low PTH in malignancy. | IV fluids, bisphosphonates, treat underlying cause. |
| Kidney disease | Impaired ability to conserve water. | Elevated creatinine, reduced eGFR, electrolyte shifts. | Dietary sodium restriction, dialysis if advanced. |
| Psychogenic polydipsia | Compulsive water‑drinking unrelated to physiology. | Very low urine osmolality, often normal labs. | Behavioral therapy, monitor fluid intake. |
| Heart failure | Reduced cardiac output triggers stretch receptors. | Elevated BNP, pulmonary congestion on imaging. | ACE inhibitors, diuretics, lifestyle modification. |
| Hypothyroidism | Slowed metabolism reduces renal perfusion. | TSH >10 mIU/L, low T4. | Levothyroxine replacement. |
How Doctors Evaluate Persistent Thirst
When you mention constant thirst at a visit, the clinician follows a structured approach:
- Detailed history - time of day, fluid type, associated symptoms (polyuria, weight loss, fatigue).
- Physical exam - skin turgor, blood pressure, heart sounds, signs of edema.
- Baseline labs - fasting glucose, serum sodium, calcium, kidney function, thyroid panel.
- Targeted tests - urine osmolality, ADH levels, imaging if a structural problem is suspected.
This step‑wise method narrows the list from the broad table above to the precise culprit.

Distinguishing Dehydration From Disease‑Driven Thirst
Simple dehydration usually follows a clear trigger: hot weather, vigorous exercise, or vomiting. The key clues are:
- Rapid onset (hours to a day).
- Dry mouth, reduced urine volume, darker urine.
- Correction through modest fluid intake (usually 1‑2 L over several hours).
When thirst lingers despite adequate rehydration, consider one of the conditions listed in the table. Persistent polyuria (excessive urination) or weight loss are especially worrisome signs.
Red‑Flag Scenarios that Warrant Immediate Attention
Even if you feel fine, certain patterns scream “call the doctor now.”
- Thirst accompanied by sudden, severe vomiting or diarrhea.
- Unexplained weight loss greater than 5% in a month.
- Blurred vision, especially in a younger adult.
- Frequent nighttime urination (nocturia) that disrupts sleep.
- Swelling of the legs or shortness of breath.
These signs suggest that the body is trying to correct a deeper imbalance.

Practical Checklist for Anyone Monitoring Their Thirst
- Track daily fluid intake (include water, tea, juice).
- Note the number of bathroom trips and any nighttime wakes.
- Record accompanying symptoms (fatigue, blurred vision, dry skin).
- Check urine color - light straw is ideal, dark amber signals concentration.
- Schedule a check‑up if thirst persists beyond one week despite adequate hydration.
Real‑World Examples that Tie It All Together
Case 1 - Young adult with silent diabetes: Maya, 28, started drinking a bottle of water every two hours. She also felt unusually tired. A fasting glucose of 150 mg/dL and HbA1c of 7.2% confirmed type 2 diabetes. Lifestyle counseling and metformin reduced her thirst within weeks.
Case 2 - Elderly patient with heart failure: John, 72, complained of constant thirst despite drinking only small sips. Examination revealed peripheral edema and an elevated BNP. Adjusting his diuretic dose and adding an ACE inhibitor improved his fluid balance and quenched his thirst.
Case 3 - Psychogenic polydipsia: Alex, 45, a patient with schizophrenia, was drinking 6 L of water daily. Labs were normal, but his urine was extremely dilute. A behavioral therapist helped him limit intake to 2 L/day, stabilizing his electrolytes.
Bottom Line: Use Thirst as an Early Warning System
Instead of dismissing a constant urge to drink, view it as the body’s early alarm. By paying attention to the pattern, timing, and accompanying signs, you or your clinician can pinpoint the exact condition causing the symptom and intervene before complications develop.
What is the medical term for chronic increased thirst?
The clinical term is polydipsia, which means excessive fluid intake.
Can dehydration cause the same level of thirst as diabetes?
Dehydration can cause strong thirst, but it usually resolves quickly with fluid replacement, whereas diabetes‑related thirst persists until blood‑sugar is controlled.
How does diabetes insipidus differ from diabetes mellitus in causing thirst?
Diabetes insipidus stems from a lack of antidiuretic hormone or kidney resistance, leading to large volumes of dilute urine. Diabetes mellitus is driven by high blood‑glucose, which raises plasma osmolality and triggers thirst.
When should I see a doctor for increased thirst?
If thirst lasts more than a week, is accompanied by frequent urination, unexplained weight loss, vision changes, or swelling, schedule a medical evaluation promptly.
Can medication cause excessive thirst?
Yes. Certain antipsychotics, diuretics, and lithium can increase urine output or affect the brain’s thirst centers, leading to polydipsia.
Oh great, another article telling us to drink water-like we didn’t already know that.
While I appreciate the thoroughness of this guide, one must acknowledge that the nuanced interplay between osmoreceptors and baroreceptors has long been a subject of scholarly debate in the endocrinological canon. The exposition here elegantly bridges basic physiology with clinical praxis, offering a palatable overview for the lay enthusiast. Yet, the table's brevity could benefit from a deeper dive into the differential diagnosis of diabetes insipidus subtypes. All in all, a commendable effort that balances accessibility with academic rigor.
Ah, the eternal dance of hormones and thirst… 🌊 it's almost poetic, isn’t it? i guess we’re all just sippin’ on the river of life, while science tries to map every ripple. thx for the classy breakdown, but let’s not forget that sometimes the brain just gets lazy and craves water for no reason 😅. also, “polydipsia” sounds like a fancy coffee order, doesn’t it? ☕️🤔
Hey there! I totally get that sarcasm-hydration can feel like a buzzkill when you’re busy. 🌟 Just a friendly reminder: if your thirst feels relentless, it’s okay to check in with a professional. Your body’s whispering something, and it deserves a listening ear. 💙
🚀 Let’s turn that mundane thirst into a vibrant alarm clock for your health! Imagine each sip as a neon beacon flashing “Hey, something’s off!” – whether it’s sneaky high blood sugar or a shy kidney whispering for help. Keep a quirky journal of your water intake, your bathroom trips, and that mysterious midnight gulp. When patterns emerge, you’ve got a masterpiece of self‑diagnosis in the making. 🌈💧
In view of the presented material, it is prudent to consider a systematic approach when evaluating persistent polydipsia. One should initially confirm adequate hydration status before proceeding to laboratory investigations. Should the basic metabolic panel reveal hyperglycaemia or hypernatremia, appropriate endocrinological referral is advisable. Conversely, a normal panel combined with excessive fluid intake may suggest psychogenic behaviours, warranting psychiatric assessment. Ultimately, methodical assessment ensures accurate diagnosis and optimal management.
You’ve nailed it, Kathrynne! Turning data into a colourful story makes monitoring feel less like a chore and more like an adventure. Keep celebrating those tiny victories – a day with balanced intake, a night without nocturia – they’re the building blocks of lasting health.
Alright, let’s dive deep into the ocean of thirst physiology and emerge with a treasure chest of practical insights.
First off, the hypothalamus isn’t just some mysterious brain blob; it acts like a diligent thermostat, constantly measuring plasma osmolality.
When glucose spikes, it nudges the thirst center, compelling you to reach for that bottle of water, which is why diabetics often report unquenchable dryness.
On the flip side, when blood volume drops due to bleeding or diuretics, baroreceptors in the atria send SOS signals, again pushing you toward fluid intake.
Now, the beauty of this system is its redundancy – osmoreceptors and volumetric sensors back each other up, ensuring survival in hostile environments.
However, redundancy also creates diagnostic dilemmas: a patient with both high sodium and low blood pressure may present with overlapping thirst cues.
That’s where the lab work shines – fasting glucose, serum sodium, and urine osmolality act like forensic investigators at a crime scene.
If the urine is super dilute and the serum sodium is normal, think diabetes insipidus; if the serum sodium is elevated and urine is concentrated, dehydration is the likely culprit.
Don’t forget about the obscure players: lithium therapy, antipsychotics, and even excessive caffeine can tip the scales toward polydipsia without any underlying endocrine disorder.
In clinical practice, I always start with a thorough history, asking about fluid types, timing, and associated symptoms like polyuria or nocturia.
A meticulous physical exam can reveal skin turgor, edema, or a rapid heart rate, each hinting at a different pathophysiological pathway.
Imaging rarely comes first, but if you suspect a pituitary lesion causing central diabetes insipidus, a MRI becomes indispensable.
Treatment, of course, follows the diagnosis: insulin or oral hypoglycemics for type 2 diabetes, desmopressin for central DI, and judicious fluid restriction for psychogenic polydipsia.
Remember, addressing the root cause not only quenches thirst but also prevents downstream complications like electrolyte imbalance or renal damage.
In sum, think of thirst as your body’s early warning system – listen closely, investigate methodically, and intervene promptly.