An Introduction to Clindamycin
As a blogger and someone interested in understanding the world of medicine, I was curious to learn more about Clindamycin. Clindamycin is a widely used antibiotic that helps treat a variety of bacterial infections. As I dived deeper into understanding how this drug works, I realized that it's important to know about its pharmacokinetics - the way Clindamycin moves through our body. In this article, I will share with you what I've learned about Clindamycin pharmacokinetics and how it works in our body. Let's get started!
Clindamycin: A Brief Overview
Clindamycin is an antibiotic in the lincosamide class, which is effective against a wide range of bacteria. It is commonly used to treat skin infections, respiratory infections, and some sexually transmitted infections. Clindamycin works by inhibiting the synthesis of bacterial proteins, which ultimately leads to the death of the bacteria. This makes it a powerful weapon in our fight against bacterial infections, but understanding how it works within our bodies is crucial for ensuring its safe and effective use.
Absorption of Clindamycin
When we take Clindamycin, it is absorbed into our bloodstream, which is the first step in its pharmacokinetics journey. The drug can be taken orally, as a capsule or liquid, or it can be administered intravenously (IV), which allows it to enter the bloodstream directly. The absorption of Clindamycin is relatively rapid, with peak plasma concentrations occurring within an hour of oral administration. However, food can slow down the absorption process, so it is usually recommended to take Clindamycin on an empty stomach.
Distribution of Clindamycin in the Body
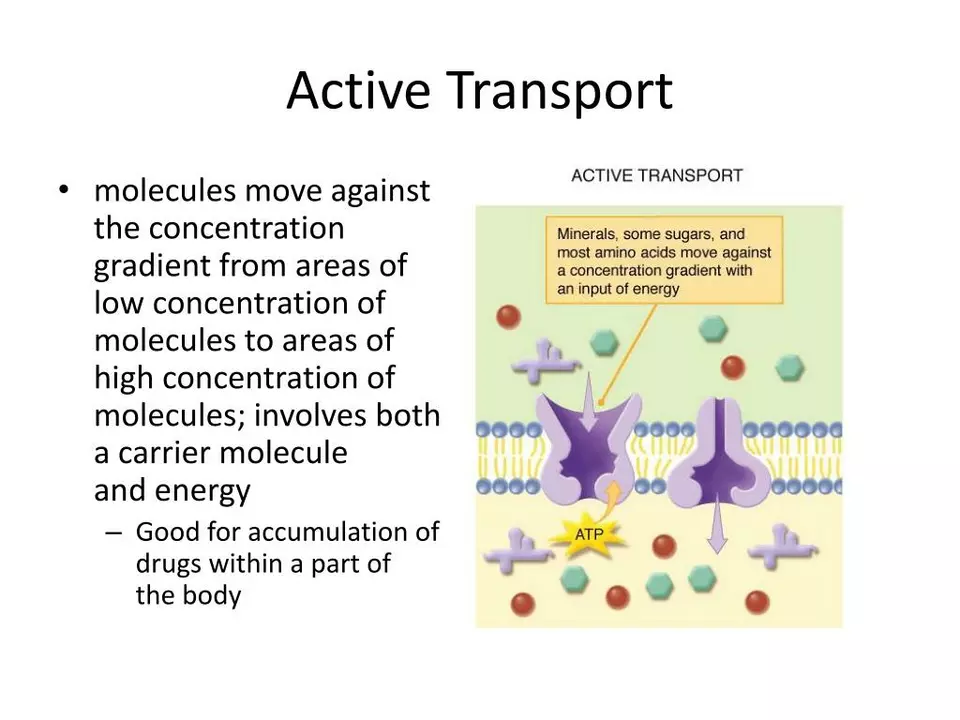
After Clindamycin is absorbed into our bloodstream, it begins to distribute throughout our body. The drug is able to penetrate various tissues, including bone, and it can even cross the placental barrier, making it an option for treating infections during pregnancy. However, Clindamycin does not penetrate the central nervous system (CNS) very well, which means it is not typically used to treat CNS infections. It's important to note that Clindamycin is highly protein-bound, which means it attaches to proteins in our blood plasma, like albumin. This can impact how the drug is distributed and eliminated from our body.
Metabolism of Clindamycin
As with most drugs, Clindamycin is metabolized in our body, primarily in the liver. Our liver enzymes break down the drug into its active metabolites, which are then able to exert their antibacterial effects. The primary metabolite of Clindamycin, N-demethylclindamycin, is also active against bacteria, although it is less potent than the parent drug. Understanding the metabolism of Clindamycin is important because it can help healthcare providers determine the appropriate dosing regimen for patients with liver function impairment.
Excretion of Clindamycin
Once Clindamycin has done its job and fought off the bacterial infection, our body needs to eliminate the drug and its metabolites. This process is known as excretion, and it primarily occurs through our kidneys. Both the parent drug and its metabolites are excreted in the urine and feces, with the majority of the drug being eliminated within 24 hours of administration. This is an important aspect of Clindamycin pharmacokinetics to be aware of, as patients with kidney impairment may require dosage adjustments to ensure the safe and effective use of the drug.
Half-Life of Clindamycin
The half-life of a drug is the time it takes for the concentration of the drug in our body to decrease by half. Clindamycin has a relatively short half-life, averaging around 2 to 3 hours. This means that after about 2 to 3 hours, the concentration of Clindamycin in our blood plasma will be around half of what it was when it was initially absorbed. Because of its short half-life, Clindamycin is typically administered multiple times per day to maintain effective concentrations in our body and fight off the infection.
Factors Affecting Clindamycin Pharmacokinetics
As with any drug, there are several factors that can affect the pharmacokinetics of Clindamycin. Some of these factors include age, weight, liver function, and kidney function. For example, elderly patients may have decreased liver and kidney function, which can impact the metabolism and excretion of Clindamycin. In such cases, healthcare providers may need to adjust the dosing regimen to ensure the safe and effective use of the drug. It's important to discuss any health concerns or conditions with your healthcare provider so they can determine the appropriate dosing regimen for you.
Conclusion
Understanding the pharmacokinetics of Clindamycin is crucial for ensuring its safe and effective use in treating bacterial infections. By knowing how the drug is absorbed, distributed, metabolized, and excreted, healthcare providers can make informed decisions when prescribing the drug and adjusting dosages for patients with specific health concerns. I hope this article has helped you better understand how Clindamycin works in our body and the importance of pharmacokinetics in the world of medicine. Stay curious and keep learning!
I find it fascinating how quickly clindamycin reaches peak plasma levels after an oral dose, usually within an hour. It’s a reminder that timing your dose relative to meals can actually matter for absorption efficiency. If you’ve ever wondered why doctors often tell you to take it on an empty stomach, it’s because food can slow that process down.
Honestly, this whole clindamycin hype feels overrated.
While the article lays out the basic pharmacokinetic steps, it conveniently omits the shadow side of pharmaceutical influence. The manufacturers fund countless studies that emphasize absorption rates, yet they rarely disclose how industry pressure shapes dosing guidelines. Behind the glossy tables lies a network of lobbyists ensuring that clindamycin stays on the market despite rising resistance patterns. Moreover, the claim that the drug penetrates bone tissue is often based on selective data, ignoring cases where patients develop deep‑site infections despite therapy. The protein‑binding characteristic, highlighted as a distribution factor, also masks the fact that free drug levels can be unpredictably low in certain populations, a detail suppressed in many clinical trials. Metabolism is described as a straightforward hepatic process, but genetic polymorphisms in CYP enzymes can dramatically alter active metabolite concentrations, leading to sub‑therapeutic effects or toxicity. The excretion section praises renal clearance, yet fails to mention how dialysis settings can trap the drug, harming patients with acute kidney injury. Even the half‑life discussion glosses over inter‑individual variability, which can stretch beyond the stated two to three hours, complicating dosing schedules. All these simplifications serve a narrative that keeps prescribers comfortable while the underlying uncertainties remain unaddressed. In an era of antibiotic stewardship, such omission is not neutral; it subtly encourages continued use without fully informing clinicians of the hidden risks. Ultimately, the article’s tidy presentation may protect readers from the messy reality of drug politics, but it does a disservice to those who rely on transparent information to make safe choices.
Picture this: you pop a clindamycin capsule, and within minutes it’s sprinting through your bloodstream like an Olympic athlete. It darts into tissues, even sneaking into bone where stubborn infections hide. The drama peaks when it meets the liver, where enzymes break it down into an active sidekick that still fights bacteria. Then, in a grand finale, the kidneys whisk it away, leaving your system clean in under a day. It’s practically a superhero storyline for a humble antibiotic.
Clindamycin’s quick absorption and short half life mean you need multiple daily doses to keep levels therapeutic
Reading this made me think of how many patients feel relieved when a drug works fast. 😊 The rapid peak concentration can really turn the tide in serious infections, especially when the bacteria are lurking deep in tissue. It’s also comforting to know the liver’s metabolite still does its job, offering a safety net if the original dose isn’t perfect. However, we must stay vigilant about liver function; the metabolite’s activity can be a double‑edged sword for those with hepatic impairment. And let's not forget the kidneys – they’re the ultimate cleanup crew, but any renal compromise needs dose tweaking. All in all, clindamycin is a solid option when used thoughtfully, and patient education about timing with meals really helps maximize its benefit. 🌟
Clindamycin, a quiet yet potent ally, reminds us that medicine often works like poetry-subtle, precise, and deeply impactful.
It’s worth noting that the drug’s high protein binding can influence both distribution and elimination, especially in patients with low albumin levels.
Clindamycin looks like a hero but forgets to mention the side effects that can ruin your gut.
Considering the drug’s ability to cross the placental barrier, clinicians should evaluate risk‑benefit ratios carefully in pregnant patients.
In my experience as a pharmacist i have observed that clindamycin does not penetrate the central nervous system well which may limit its use in certain infections . Also the dosage might need adjustment in elderly patients due to decreased hepatic and renal function . I would also like to mention that while the drug is generally well tolerated , there is a risk of C. difficile colitis that clinicians must monitor for . This is especially important when prescribing broad‑spectrum antibiotics like clindamycin . The half‑life variability also means that some patients may require more frequent dosing to maintain therapeutic levels .
Great overview! Remember to individualize dosing based on liver and kidney function; a small tweak can make a huge difference in outcomes.
Clindamycin’s quick absorption is useful but don’t forget to time it right with meals to avoid slower uptake.
Clindamycin, a widely used antibiotic, is effective against a broad spectrum of bacteria, and its pharmacokinetic profile includes rapid absorption, extensive tissue distribution, hepatic metabolism, and renal excretion; the drug’s high protein binding influences its distribution, while its short half‑life necessitates multiple daily doses to maintain therapeutic concentrations; clinicians should adjust dosing in patients with hepatic or renal impairment, and be aware of potential adverse effects such as C. difficile infection.
When you’re dosing clindamycin, keep an eye on liver enzymes – they’ll tell you if the drug’s being processed safely.
Clindamycin works well for skin infections, but always check kidney function before prescribing.
Accurate dosing requires consideration of both hepatic metabolism and renal clearance to avoid sub‑therapeutic exposure.
Clindamycin, as a staple of Anglo‑American medicine, exemplifies the brilliance of our pharmaceutical heritage; its pharmacokinetics are well‑studied, its efficacy proven, and any criticism from foreign sources is often misguided; the drug’s rapid absorption, reliable tissue distribution, and predictable elimination make it indispensable, and attempts to undermine its reputation should be dismissed as anti‑British sentiment.