Bioavailability Issues: Why Some Medications Don't Work Like They Should
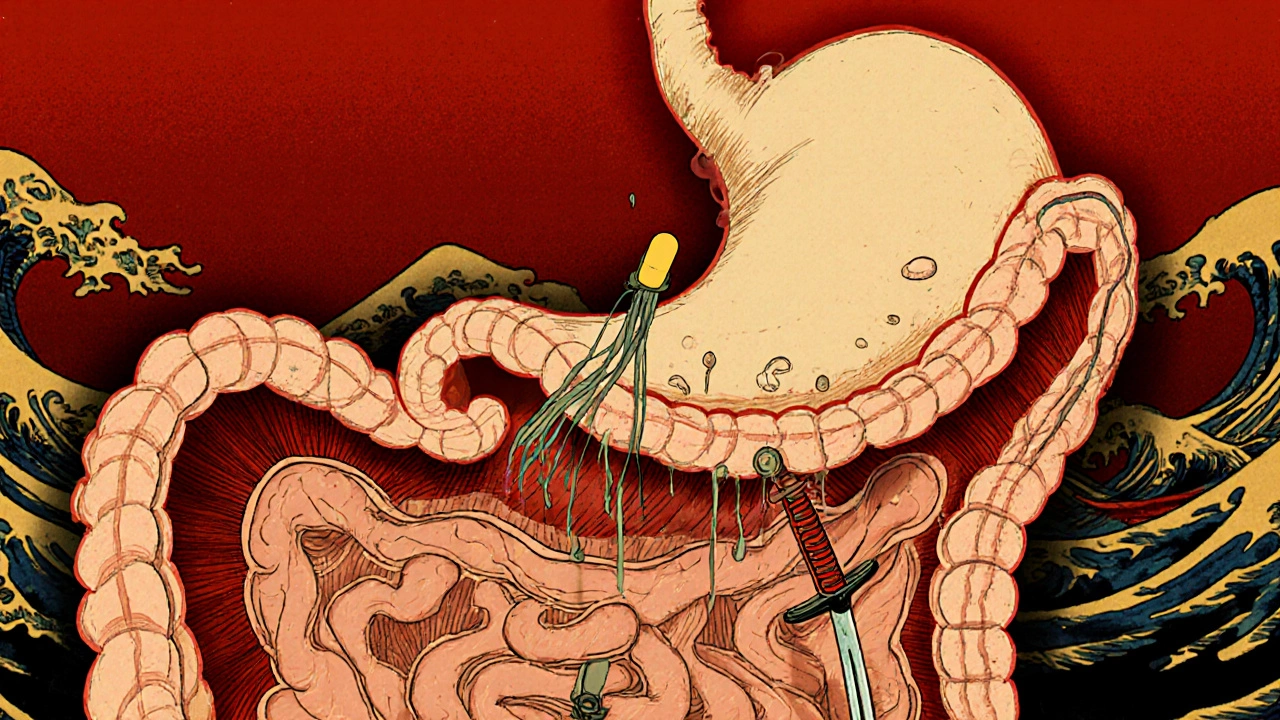
When a drug doesn’t do what it’s supposed to, it’s often not because it’s weak—it’s because your body can’t absorb it properly. This is called bioavailability issues, the percentage of a drug that enters circulation and has an active effect. Also known as drug absorption efficiency, it’s the hidden factor that decides whether your pill works, barely works, or doesn’t work at all. You might take the same dose as someone else, but if your stomach acid, gut bacteria, or liver enzymes handle it differently, the result can be wildly different.
That’s why generic drugs, lower-cost versions of brand-name medications sometimes feel less effective—even though they contain the same active ingredient. The FDA allows generics to vary in bioavailability by up to 20% compared to the original. For most drugs, that’s fine. But for narrow-therapeutic-index drugs like warfarin or levothyroxine, even a small drop in absorption can cause serious side effects or treatment failure. This isn’t about quality control—it’s about how the drug is formulated: the fillers, coatings, and how fast it dissolves all matter. A pill that dissolves too slowly might never reach the right part of your gut. One that dissolves too fast might get broken down before it can be absorbed.
pharmacokinetics, how your body moves a drug through absorption, distribution, metabolism, and excretion is the science behind why bioavailability varies. Food, timing, other meds, and even your genetics can change it. For example, taking a statin with grapefruit juice can spike blood levels dangerously. Taking an antibiotic on an empty stomach might make it work better—or worse, depending on the drug. And when you’re on multiple meds, interactions can block absorption entirely. That’s why some people feel fine on a drug for months, then suddenly it stops working—something in their routine changed.
These issues aren’t rare. They show up in real cases: a patient on thyroid meds who switches to a cheaper generic and starts feeling fatigued again. Someone on epilepsy drugs who has a seizure after changing pharmacies. A person taking a supplement like garlic extract, a natural compound often marketed for heart health that’s poorly absorbed unless it’s aged or enteric-coated. These aren’t accidents. They’re predictable outcomes of poorly understood bioavailability.
What you’ll find in this collection isn’t just theory. It’s real-world fixes. You’ll see how hospital formularies choose generics based on bioavailability data, why some supplements like Lasuna garlic extract are formulated differently to boost absorption, and how drug interactions can sabotage even the best-intentioned treatment. You’ll learn how to spot when a medication isn’t working because of absorption—not because it’s ineffective. And you’ll understand why sometimes, the difference between a drug that works and one that doesn’t comes down to something as simple as when you took it, what you ate, or which pharmacy filled it.
Gastrointestinal Medications: Why Absorption Issues Ruin Effectiveness
Many gastrointestinal medications fail to work because of absorption issues caused by gut physiology, food interactions, and disease. Learn why your pills might not be working and what you can do about it.
read more