
When your pharmacy hands you a new pill that looks completely different from the one you’ve been taking for years, it’s easy to assume it’s the same thing. After all, the label says the same active ingredient. But if you’ve ever felt off after a switch - sudden anxiety, brain fog, seizures, or unexplained fatigue - you’re not imagining it. For some people, switching between generic versions of the same drug isn’t just a paperwork change. It can trigger real, measurable side effects.
Why a Generic Isn’t Always the Same
The FDA says generics are bioequivalent to brand-name drugs. That means they must deliver 80% to 125% of the active ingredient into your bloodstream compared to the original. Sounds tight, right? But here’s the catch: that 45% window - from 80% to 125% - is the total possible spread between two different generics of the same drug. For most medications, that’s fine. For others, it’s dangerous. Drugs with a narrow therapeutic index (NTI) are the real concern. These are medications where even a small change in blood levels can cause treatment failure or toxicity. Think: seizure meds like phenytoin, thyroid hormone levothyroxine, blood thinners like warfarin, and immunosuppressants like tacrolimus. In these cases, a 10% drop in absorption might mean your seizures return. A 10% rise could mean internal bleeding. And it’s not just about the active ingredient. Generics can differ in fillers, coatings, and how the drug is released over time. One manufacturer might use a slow-release bead system. Another might crush and re-formulate the same powder. For extended-release drugs like Adderall XR or bupropion XL, those differences can change how quickly the drug hits your brain - and how long it lasts.Who’s Most at Risk?
Not everyone reacts to generic switches. But certain groups are far more likely to notice a difference:- People with epilepsy, especially those with hard-to-control seizures
- Patients on thyroid medication - even tiny changes can throw off metabolism, heart rate, and mood
- Those taking anticoagulants like warfarin - INR levels can swing dangerously
- Organ transplant recipients on tacrolimus or cyclosporine
- People with ADHD on extended-release stimulants - many report sudden loss of focus or new anxiety
- Individuals with CYP2D6 poor metabolizer genetics - they process certain antidepressants and pain meds differently
Real Stories, Real Consequences
Reddit threads like “Generic Adderall Switch Ruined My Life” have over 800 comments. People describe waking up with panic attacks they’d never had before. Others say their focus vanished overnight. One woman wrote: “I was stable for five years on the old generic. Switched to a new one. Three days later, I couldn’t get out of bed. My doctor said it was ‘all in my head.’” A 2023 hospital review of 1,437 patients found that 20% of those who were accidentally given duplicate generics - because they didn’t recognize the new pill - ended up with side effects. One case led to serotonin syndrome, requiring emergency care. Neurologists aren’t ignoring this. A 2021 survey of 147 specialists found that 68.7% believed switching generic antiepileptics increased seizure risk. Over 40% had seen it happen in their own clinics.
What the FDA Says vs. What Doctors See
The FDA maintains that no clinical evidence shows generics cause problems in the general population. But that’s not the full picture. The FDA’s standards are based on population averages. They don’t account for individual sensitivity. Dr. Lenard A. Guttman, a clinical pharmacy professor, says 30-40% of his ADHD patients notice clear differences after a generic switch - often within 24 to 72 hours. That’s not anecdotal. That’s clinical observation. The American Academy of Neurology and the American Society of Health-System Pharmacists have both issued warnings. In January 2024, the latter released new guidelines listing 17 specific drugs where automatic substitution should be avoided. These include bupropion XL, tacrolimus, and phenytoin.How to Protect Yourself
You don’t have to accept random pill changes as normal. Here’s what you can do:- Check the pill. Note the shape, color, and imprint code (like “A 10” or “V 30”). Write it down. If it changes, ask why.
- Ask for the manufacturer name. When you pick up your prescription, ask the pharmacist: “Which company made this?” Some generics are made by Teva, Mylan, or Sandoz. Stick with the one that works.
- Request “Dispense As Written”. Tell your doctor you want the prescription marked DAW-1. That legally prevents the pharmacy from switching it without your consent.
- Keep a log. Track your symptoms, dosage, and manufacturer name every time you refill. Use a notebook or your phone. If you feel worse after a switch, you’ll have proof.
- Don’t wait. If you notice new side effects or loss of effectiveness within 3 days of a refill, call your doctor. Don’t assume it’s “just adjustment.”
Why Do These Switches Keep Happening?
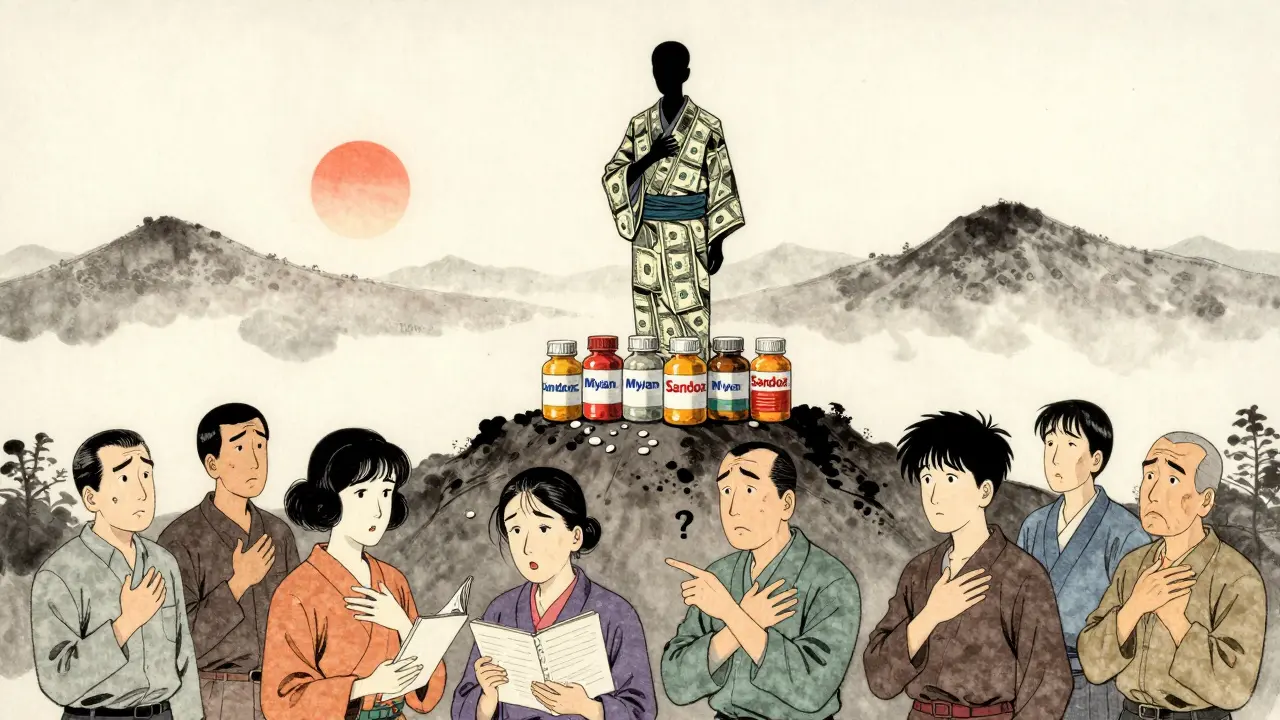
It’s not about your health. It’s about money. Pharmacy benefit managers (PBMs) - companies like CVS Caremark and Express Scripts - control which generics pharmacies stock. They get rebates from manufacturers. The higher the rebate, the more they push that brand. So pharmacies switch you every few months to whichever generic offers the biggest kickback. A 2022 Senate investigation found PBMs change preferred generic manufacturers an average of 4.7 times per year per drug. Levothyroxine alone has 12 different generic makers. That means if you’re on thyroid meds, you might get a different pill every 2-3 months. And it’s not just you. Over 187 million Americans are affected. The system is built to save money - but the hidden cost? Hospitalizations, ER visits, lost workdays. One 2023 study estimated preventable side effects from generic switching cost the U.S. system $2.1 billion a year.What’s Changing?
Good news: change is coming - slowly. In 2023, Medicare Part D rules now limit generic switches to just twice a year. That’s a start. The FDA’s Complex Generic Products Initiative is developing better testing methods for tricky drugs like inhalers and topical creams. And in 2024, new research confirmed that people with certain genetic profiles (like CYP2D6 poor metabolizers) are 4.2 times more likely to fail on switched antidepressants. More doctors are starting to ask for DAW-1 codes. More pharmacists are willing to hold a specific generic if you ask. It’s not universal - but it’s growing.Bottom Line
Generics save billions. That’s good. But they’re not all created equal - especially for high-risk drugs. If you’re on a narrow therapeutic index medication, don’t treat a pill change like a routine refill. Pay attention. Speak up. Document everything. Your body knows when something’s off. Trust it. And don’t let a rebate form decide what’s safe for you.Can switching between generic drugs really cause side effects?
Yes, for certain medications - especially those with a narrow therapeutic index like antiepileptics, thyroid hormones, blood thinners, and some psychiatric drugs. Even small differences in how the drug is absorbed can lead to loss of effectiveness or new side effects like anxiety, fatigue, or seizures. While the FDA considers generics bioequivalent, real-world patient reports and clinical studies show that some individuals are sensitive to formulation changes.
Which generic drugs are most likely to cause problems when switched?
The highest-risk categories include: antiepileptic drugs (like phenytoin and divalproex), levothyroxine (thyroid hormone), warfarin (blood thinner), tacrolimus and cyclosporine (immunosuppressants), and extended-release ADHD medications like Adderall XR and Vyvanse. These drugs have little room for error - even minor changes in blood levels can cause serious consequences.
How can I tell if my generic medication has been switched?
Check the physical appearance: color, shape, size, and the imprint code (letters/numbers on the pill). If it looks different from your last refill, it’s likely a different manufacturer. Ask the pharmacist for the manufacturer name - it’s usually listed on the bottle or packaging. Keep a record of what each pill looks like so you can spot changes quickly.
Can I ask my doctor to prevent generic switches?
Yes. Ask your doctor to write “Dispense As Written” or “DAW-1” on your prescription. This legally prevents the pharmacy from substituting a different generic without your consent. This is especially important for high-risk medications. Many doctors are willing to do this if you explain your concerns.
Why do pharmacies keep switching my generic medication?
Pharmacy benefit managers (PBMs) - like CVS Caremark or Express Scripts - control which generics are stocked and get rebates from manufacturers. They switch to whichever generic offers the highest rebate, often every few months. It’s not about your health - it’s about profit. This practice affects millions of people and can lead to unstable drug levels in the body.
What should I do if I feel worse after switching to a new generic?
Don’t ignore it. Contact your doctor immediately. Note the date of the switch, the new pill’s appearance, and your symptoms. Keep a log. If you’re on a high-risk medication, your doctor may need to switch you back to the previous version or request a specific manufacturer. In some cases, you may need to pay more out-of-pocket to get the formulation that works - but it’s safer than risking side effects.
They call it bioequivalent but never ask if your body agrees. I switched generics for my seizure med and woke up feeling like my brain had been rewired by a drunk electrician. Three days of panic attacks, zero help from my doctor who said 'it's just stress.' I had to fight for three months to get my old one back. Now I take a photo of every pill before I swallow it. Trust your body more than the FDA's math.
My cousin in Lagos was on levothyroxine for years - stable, healthy, working as a teacher. Then the pharmacy switched her generic without telling her. She started losing weight, trembling, crying for no reason. Took her two months and three hospital visits to figure out it was the pill. Now she brings her own medication from Nigeria when she travels. We need to stop treating human bodies like interchangeable parts. Your life isn't a cost-cutting spreadsheet.
so like… the fda says its the same but people feel different?? wow. mind blown. i mean… if your brain says its wrong… maybe its wrong? who knew. also why do we let corporations decide what medicine we get? capitalism is a drug too. and its side effects are… us.
It’s fascinating how we’ve outsourced our health to algorithms and rebate structures. We’ve turned medicine into a commodity traded on invisible markets, where the human body becomes a variable in a profit equation. The FDA’s bioequivalence standard assumes a statistical average - but we are not averages. We are individuals with unique metabolisms, genetic expressions, and neurological sensitivities. The fact that we accept this as normal speaks to a deeper cultural failure: we’ve stopped seeing ourselves as sentient beings and started seeing ourselves as data points. If your thyroid medication changes every 60 days, you’re not being treated - you’re being managed. And management is not care.
Why are we letting foreign manufacturers make our meds? If this was a car or a phone, we’d ban it. America makes better pills. We should only allow US-made generics. No more Teva, no more Mylan - just American quality. This isn’t about money, it’s about national security. Your brain is on foreign soil.
This is a critical public health issue that deserves far more attention. The data is clear: for narrow therapeutic index drugs, variability in formulation directly correlates with adverse outcomes. The FDA’s current testing protocols are outdated and fail to account for pharmacokinetic differences in extended-release formulations. I urge all patients on these medications to document every switch, request DAW-1, and report adverse events to MedWatch. Systemic change requires collective documentation.
This is why I always ask for the manufacturer name - and I keep a little notebook with pill photos. 📸 I’ve been on warfarin for 12 years. One switch = INR spike to 7.2. Emergency room. ICU. Nearly bled out. Now I tell my pharmacist: 'If it doesn’t look like the last one, I’m walking out.' It’s not rude - it’s survival. You’re not being difficult. You’re being smart. 💪❤️
this is all fake news made by big pharma to sell more brand name drugs the fda is not lying its just that people are weak and cant handle change the real problem is you people think your body is special when its not everyone gets the same pill in china and they dont have seizures so stop being dramatic
There’s a quiet revolution happening in pharmacy advocacy. More patients are refusing automatic substitution. More doctors are writing DAW-1. More pharmacists are starting to push back on PBMs. It’s not easy - but it’s working. I had to pay $80 extra for my old Adderall XR generic last month. Worth every penny. My focus came back in 48 hours. Your health isn’t a line item. It’s your life. Fight for it - politely, persistently, and with receipts.
Changed generics last month. Felt weird. Didn’t say anything. Then it got worse. Called doctor. Got my old one back. No drama. Just… don’t ignore it. Your body talks. Listen.
generic switch bad? maybe you just need to stop being so sensitive
Oh wow. So the government lets a corporation decide what’s in my brain? How quaint. I’m sure the board meeting where they picked Teva over Mylan had a lovely view of the ocean. Next time I’ll just ask my pill if it’s having a good day.
I’m a doctor. And I can tell you - this is all just anxiety. People see a different color pill and panic. It’s psychosomatic. If you’re not a genius with a PhD in pharmacology, you shouldn’t be second-guessing science. Just take the pill and be grateful it’s cheap.
Respected colleagues, this matter pertains to a significant concern in clinical pharmacology. The variance in bioavailability among generic formulations, particularly for drugs with narrow therapeutic indices, is empirically documented in peer-reviewed literature. It is imperative that healthcare providers, pharmacists, and patients engage in transparent communication regarding formulation changes. I recommend institutional protocols to mandate manufacturer disclosure and patient education. The ethical obligation to patient safety supersedes cost-efficiency metrics.
so i switched generics for my antidepressant and felt like a zombie for a week. told my dr. she said 'maybe you need more coffee?' 🤡 i wrote down the pill code and now i only take the one that says 'A 215'. no one believes me but i know. my brain remembers what my doctor forgot.
They call it bioequivalent but never ask if your body agrees. I switched generics for my seizure med and woke up feeling like my brain had been rewired by a drunk electrician. Three days of panic attacks, zero help from my doctor who said 'it's just stress.' I had to fight for three months to get my old one back. Now I take a photo of every pill before I swallow it. Trust your body more than the FDA's math.