
Most people don’t realize it, but when they scroll through Instagram or watch a TikTok video about managing diabetes, they’re already part of a new kind of healthcare system. Social media education isn’t just for schools anymore-it’s becoming a powerful tool for patient education. In 2026, patients are turning to platforms like TikTok, Instagram, and YouTube to learn how to take their medications, understand side effects, or even manage chronic conditions like hypertension or asthma. This isn’t random. It’s a shift driven by real behavior, real data, and real results.
Back in 2018, if you asked a patient where they learned about their condition, most would say, "My doctor." Today? A 2025 survey by HealthTech Insights found that 61% of adults with chronic illnesses turned to social media first before contacting their provider. Why? Because it’s faster, more relatable, and often more visual. A 60-second video showing someone injecting insulin with simple step-by-step captions sticks better than a 12-page pamphlet.
Why Social Media Works for Patient Education
Think about how you learn best. For many, it’s not reading a textbook. It’s watching someone do it, hearing from someone who’s been there, or seeing a quick demo you can pause and replay. That’s exactly what social media offers.
Platforms like YouTube and Instagram have become go-to sources for health content. YouTube’s 2.7 billion logged-in users mean there’s an audience for nearly every condition. Educational videos on managing Type 2 diabetes now average 18.4 minutes of watch time per viewer-up from 13.1 minutes in 2023. That’s not just views. That’s engagement. People are watching long enough to absorb information.
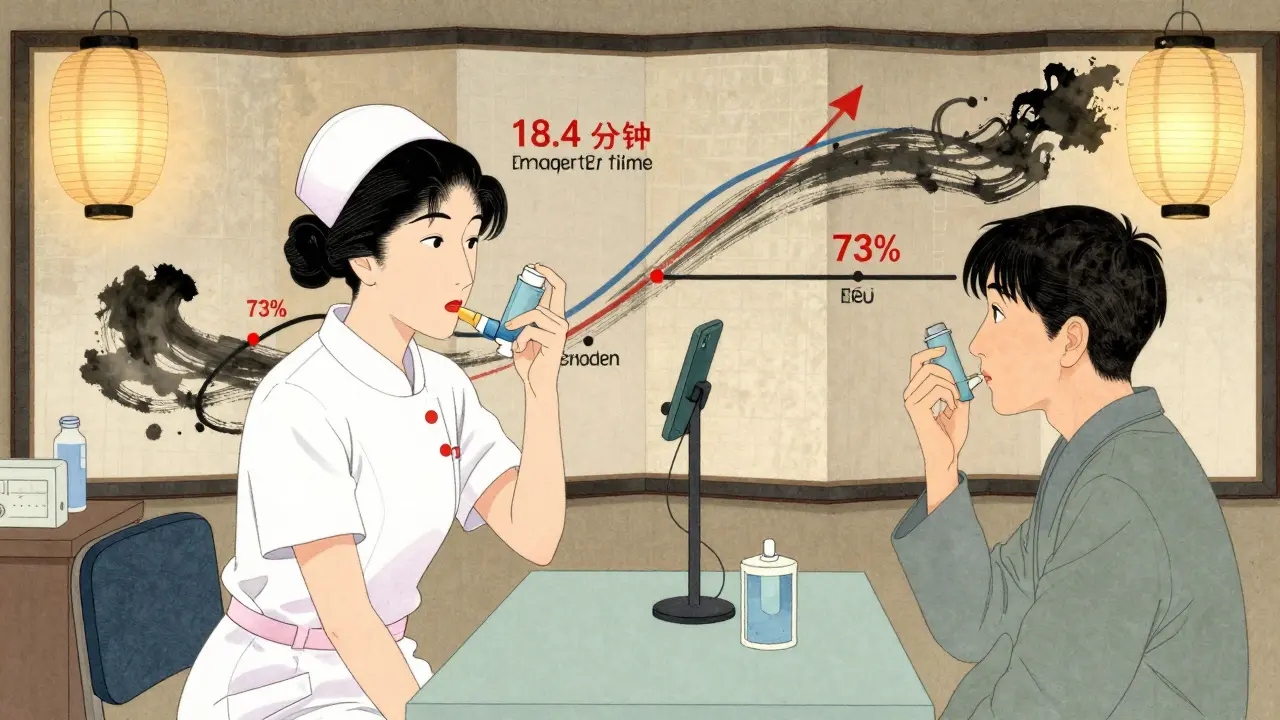
Instagram Reels and TikTok videos under 90 seconds are even more effective. A 2025 study from the New Zealand Health Research Institute showed that short-form videos explaining how to use an inhaler had a 73% retention rate among patients aged 18-35. Compare that to printed instructions, where only 29% of patients recalled the correct technique after one week.
And it’s not just about watching. It’s about interaction. When a patient comments, "I tried this and my blood sugar dropped," or "Does this work for kids?"-they’re not just asking a question. They’re building a community. These conversations create trust. And trust leads to better adherence.
Which Platforms Are Actually Used by Patients?
Not all platforms are created equal when it comes to health education. Here’s what’s working in 2026:
- YouTube: Best for detailed, long-form content. Patients use it to watch full tutorials on managing COPD, understanding lab results, or learning physical therapy exercises. Channels run by accredited clinics see 4x more shares than generic ones.
- Instagram: Ideal for visual learners. Infographics on medication schedules, Reels showing how to use an EpiPen, and Stories with countdowns for refill reminders perform best. Posts with captions and text overlays get 58% more engagement.
- TikTok: The fastest-growing platform for health education. Hashtags like #MedicationTips and #ChronicIllnessJourney have over 2.1 billion combined views. A 2025 analysis found that 68% of patients under 30 learned about a new drug from a TikTok video before their doctor mentioned it.
- Facebook Groups: Still powerful for older adults and caregivers. Groups like "Living with Heart Failure" or "Parents of Kids with Asthma" provide peer support, shared experiences, and moderated Q&A sessions. These groups have 3x higher retention than email newsletters.
- LinkedIn: Less for patients, more for providers. Doctors, nurses, and pharmacists use it to share research, guidelines, and patient education tools. It’s where professional networks exchange resources.
One key insight: patients don’t use one platform. They move across them. A teen with asthma might see a TikTok video, then search Instagram for more tips, join a Facebook group for parents, and watch a YouTube demo before their next appointment. This multi-touch journey is now the norm.
Real Examples That Are Making a Difference
In Auckland, a local pharmacy launched a TikTok series called "Medication Minute" in late 2024. Each 60-second video breaks down one common drug-how to take it, what to avoid, what side effects mean. Within six months, they saw a 41% drop in medication-related calls to their helpline. Why? Because patients weren’t confused anymore.
At Waikato Hospital, nurses started posting Instagram Stories every Tuesday showing real patients (with consent) talking about their treatment journeys. One post showed a woman explaining how she learned to use her insulin pump after watching a video. That single Story got 14,000 views and 872 saves. The hospital’s patient satisfaction scores for diabetes education jumped 22% in three months.
A small clinic in Christchurch partnered with high school students to create YouTube videos explaining asthma triggers in simple language. The students used their phones, edited on free apps, and posted under the clinic’s account. The videos went viral locally. Enrollment in their asthma management program increased by 35% in six months.
These aren’t flashy campaigns. They’re simple, human, and consistent. The common thread? Real people. Real stories. No jargon.
What Goes Wrong? Common Pitfalls
Not every social media effort works. Some fail because they treat it like advertising.
One hospital posted polished ads with stock photos of smiling patients and said, "Our new diabetes program is amazing!" The engagement? Barely 120 likes. Another clinic tried using AI-generated videos to explain hypertension. Patients commented, "This doesn’t feel real." Trust dropped.
Here’s what goes wrong:
- Using too much medical jargon
- Only posting from staff, never from patients
- Ignoring comments or not responding to questions
- Posting inconsistently-once a month doesn’t build habit
- Not using captions or subtitles (44% of viewers watch without sound)
And then there’s misinformation. A 2025 report from the New Zealand Medical Council found that 31% of patients had encountered false claims about medications on social media. That’s why credible sources must step in. Hospitals and pharmacies that verified their profiles (blue check, official website link, clear bio) saw 67% fewer false claims shared about their services.

How to Start-Step by Step
If you’re a healthcare provider, clinic, or pharmacy wondering where to begin, here’s how:
- Pick one platform. Don’t try to do everything. Start with the one your patients already use. For under-40s? TikTok or Instagram. For over-50s? Facebook or YouTube.
- Find your first topic. What’s the most common question you get? "How do I take this pill?" "What foods affect my blood pressure?" Start there.
- Create a 60-second video. Use your phone. No fancy gear needed. Show the medication, the action, the timing. Add text captions. Keep it simple.
- Post and respond. Don’t just upload. Answer comments. Ask questions back. Build conversation.
- Do it again. Consistency beats perfection. Three posts a month is better than one perfect one every three months.
Track what works. Use free tools like Instagram Insights or YouTube Analytics. See which videos get saved, shared, or commented on. That’s your signal: this matters to people.
The Bigger Picture
This isn’t just about posting videos. It’s about changing how healthcare works. Social media education turns patients from passive recipients into active participants. When someone learns how to use their inhaler from a peer on TikTok, they’re not just following instructions-they’re becoming part of a support network.
By 2027, the World Health Organization predicts that over half of all patient education will happen through digital platforms before a single clinic visit. That’s not a threat. It’s an opportunity.
Healthcare doesn’t need to be perfect. It needs to be present. And social media is where people are already looking.
Can social media replace doctor visits for patient education?
No, social media can’t replace doctor visits. But it can dramatically improve what happens before and after. Patients who learn about their condition through verified social content arrive at appointments better prepared, ask smarter questions, and follow treatment plans more consistently. It’s not a replacement-it’s a powerful support layer.
Are TikTok and Instagram safe for medical advice?
It depends on who’s posting. Unverified influencers can spread dangerous misinformation. But verified accounts from hospitals, pharmacies, and licensed health professionals are reliable. Look for clear credentials in the bio, links to official websites, and consistent messaging with trusted sources like the Ministry of Health or WHO. Always cross-check critical advice with your provider.
What kind of content works best for older patients?
Older patients respond best to clear, slow-paced videos on YouTube or Facebook. Use large text, simple language, and real-life scenarios-like showing how to open a pill bottle or set a medication alarm. Facebook Groups are especially effective because they offer community support, which many older adults value more than flashy visuals.
How do I know if my social media content is accurate?
Always base your content on official guidelines from the Ministry of Health, Pharmac, or peer-reviewed journals. Have a pharmacist or clinician review your scripts before posting. Include sources in captions (e.g., "Based on NZ Guidelines 2025"). Avoid absolute statements like "This always works." Instead, say "This works for most people."
Do I need a big team to run social media for patient education?
No. Many small clinics succeed with just one person managing content for one platform. A nurse or pharmacist can film a 60-second video on their phone during a quiet moment. The key isn’t resources-it’s consistency and authenticity. One real person, one clear message, posted weekly, beats a flashy campaign no one watches.
What’s the biggest mistake clinics make?
Treating social media like an ad campaign. If your posts look like commercials-stock photos, generic slogans, no real patients-you’ll be ignored. The most successful content feels like a conversation. It’s a patient sharing their story. A nurse answering a question. A pharmacist showing how to use a device. Real. Human. Relatable.
Patients aren’t waiting for brochures anymore. They’re scrolling. And if you’re not there with clear, honest, helpful information, someone else will be.