
MAOI-Opioid Interaction Risk Calculator
Medication Selection
Risk Assessment Results
Please select medications and click "Calculate Risk" to see results.
- Never take tramadol, meperidine, or methadone while on an MAOI
- Wait 14 days after stopping irreversible MAOIs before using opioids with serotonergic effects
- Carry a medical alert card listing your medications
- Always inform healthcare providers about your MAOI use
Why Mixing Opioids and MAOIs Can Kill You
It sounds like something out of a medical thriller: you take a common painkiller, and your body goes into overdrive-temperature spikes to 107°F, muscles lock up, seizures start. This isn’t fiction. It’s what happens when certain opioids mix with MAOIs, a class of antidepressants still used for treatment-resistant depression. The interaction isn’t just risky-it’s deadly. And it’s happening more often than you think.
The first documented death from this combo happened in 1964. A patient on iproniazid, one of the earliest MAOIs, was given meperidine (Demerol) for pain. Within hours, they died from a massive serotonin surge. Since then, over 127 confirmed cases of serotonin syndrome from this interaction have been recorded worldwide. At least 89 of those cases ended in death. And yet, doctors still prescribe these drugs together-sometimes because they don’t know the risk, sometimes because they think the patient’s pain is too severe to avoid opioids.
How the Interaction Works
MAOIs work by blocking monoamine oxidase enzymes, which normally break down serotonin, norepinephrine, and dopamine. That’s why they help with depression-these mood-boosting chemicals stick around longer. But when you add certain opioids, you’re essentially pouring gasoline on a fire.
Drugs like tramadol, meperidine, and methadone don’t just relieve pain. They also increase serotonin in your brain. Tramadol blocks serotonin reuptake. Meperidine forces serotonin out of nerve cells. Methadone does both. When MAOIs are already preventing serotonin from being cleared, these opioids flood the system. The result? Serotonin syndrome-a condition where your nervous system goes haywire.
But it’s not just serotonin. Some opioids, like fentanyl, trigger norepinephrine release. MAOIs stop your body from breaking down norepinephrine too. That combination can spike your blood pressure to dangerous levels-240/140 mmHg or higher-leading to stroke, heart attack, or organ failure.
Which Opioids Are Most Dangerous?
Not all opioids are created equal when it comes to MAOI interactions. Here’s the breakdown:
- Meperidine (Demerol): The deadliest. Responsible for 37 documented deaths between 1960 and 2010. It’s so dangerous that the FDA explicitly bans it for anyone on MAOIs.
- Tramadol: The most common culprit today. Even though it’s often called a "non-narcotic," it’s just as risky as traditional opioids when mixed with MAOIs. Over 68 cases of serotonin syndrome have been tied to this combo since 2010.
- Methadone: Moderate risk. It affects serotonin and has NMDA-blocking effects that can worsen CNS depression.
- Morphine, oxycodone, hydromorphone: Lower risk-but still dangerous. They don’t directly boost serotonin much, but they can still trigger reactions in sensitive individuals.
- Buprenorphine: The safest option. Used in emergency settings for MAOI patients because it has minimal serotonergic activity.
Even reversible MAOIs like moclobemide aren’t safe. There are documented cases of serotonin syndrome with tramadol and moclobemide at normal doses. There’s no such thing as a "safe" opioid for someone on an MAOI-except buprenorphine, and even that needs careful dosing.

How Long Should You Wait After Stopping an MAOI?
Many people think if they stop their MAOI a few days before surgery or a new pain prescription, they’re fine. They’re wrong.
Irreversible MAOIs like phenelzine (Nardil) and tranylcypromine (Parnate) permanently disable the enzyme. Your body has to grow new enzymes to replace them. That takes about 14 days. The FDA and every major medical guideline-American Psychiatric Association, Mayo Clinic, American Society of Anesthesiologists-agree: you must wait at least two weeks after stopping an MAOI before starting any opioid with serotonergic effects.
Reversible MAOIs like moclobemide clear faster. A 24-hour wait is usually enough. But here’s the catch: most doctors don’t know which type their patient is on. And many patients don’t even realize they’re on an MAOI-some are prescribed for pain, not depression.
What Happens When You Mix Them?
Serotonin syndrome doesn’t sneak up. It hits fast. Symptoms usually appear within 1 to 6 hours after taking the opioid. They include:
- High fever (104°F or higher)
- Shivering, muscle rigidity (so severe you can’t move)
- Fast heart rate, high blood pressure
- Confusion, hallucinations, seizures
- Loss of coordination, diarrhea
One Reddit user, u/ChronicPainWarrior, described their experience: "I got tramadol for a toothache. Two hours later, I couldn’t breathe. My body was locked. I was burning up. I ended up in ICU for three days."
In hospitals, these cases are emergencies. Treatment includes benzodiazepines to calm the nervous system, cooling blankets for fever, and cyproheptadine-a serotonin blocker-to reverse the reaction. But if treatment is delayed, death can happen within 12 hours.
Why Is This Still Happening?
You’d think after 60 years of warnings, this wouldn’t happen. But it does.
A 2022 study in JAMA Internal Medicine found that 4.3% of people on MAOIs were still prescribed contraindicated opioids within 14 days of starting the antidepressant. That’s about 11,200 dangerous prescriptions every year in the U.S. alone.
Why? Three big reasons:
- Tramadol is mislabeled. Many patients and even some doctors think it’s "not an opioid" because it’s sometimes sold as a non-narcotic. It’s not. It’s an opioid with serotonin effects.
- Doctors don’t ask. Primary care providers often don’t know their patient is on an MAOI. Mental health records aren’t always shared with pain clinics or ERs.
- Patients don’t speak up. Many don’t realize MAOIs are dangerous with pain meds. They don’t carry warning cards. They don’t mention them unless asked.
Even with electronic health records that flag these interactions, 14.3% of alerts are overridden by clinicians. That’s over 1,200 times a year someone ignores a life-saving warning.
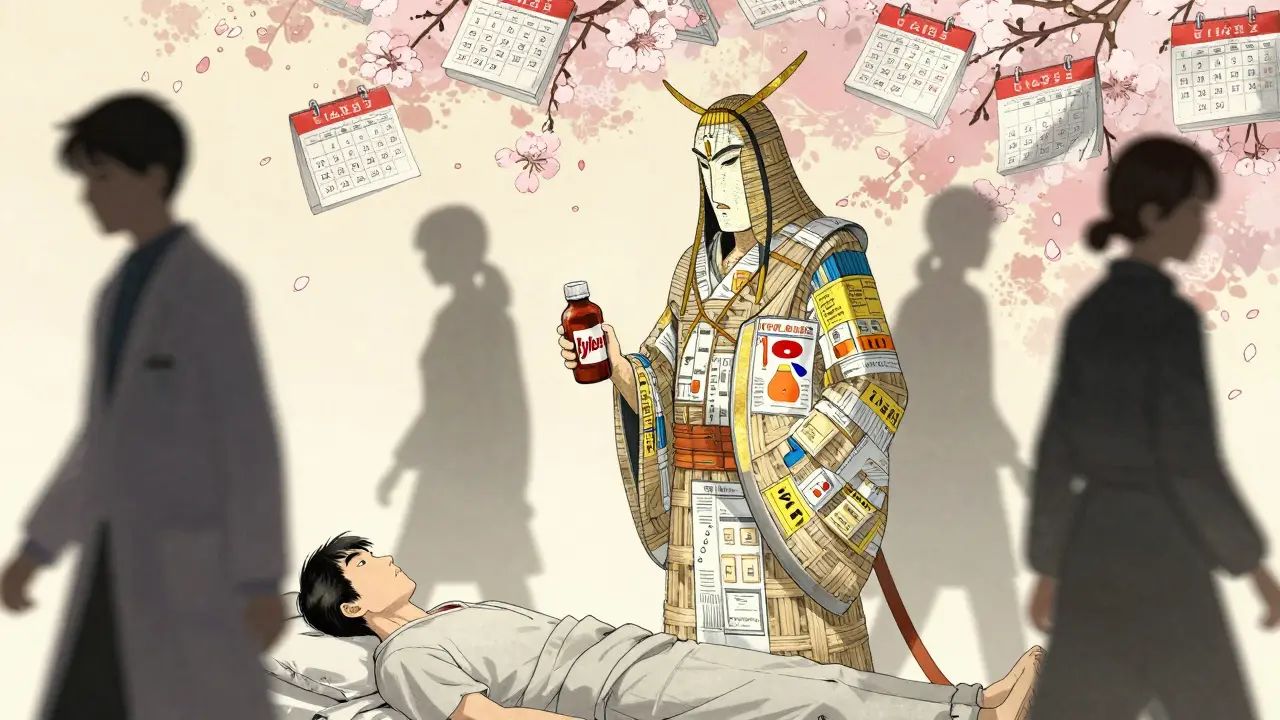
What Should You Do If You’re on an MAOI?
If you’re taking an MAOI, here’s what you need to do right now:
- Know your drug. Is it phenelzine, tranylcypromine, isocarboxazid, or selegiline? These are MAOIs. If you’re unsure, check the pill bottle or ask your pharmacist.
- Never take tramadol, meperidine, methadone, or dextromethorphan. These are absolute no-gos. Even over-the-counter cough syrups with dextromethorphan can trigger a reaction.
- Carry a warning card. The National Alliance on Mental Illness offers free wallet cards listing contraindicated drugs. 78% of patients who carry them say it’s saved them from dangerous prescriptions.
- Tell every doctor, dentist, and ER staff. Say it clearly: "I’m on an MAOI. I cannot take tramadol, meperidine, or any opioid with serotonin effects."
- Wait 14 days after stopping MAOI before any opioid. Don’t guess. Don’t assume. Wait the full two weeks.
For pain, stick to safer options: acetaminophen (Tylenol), ibuprofen (Advil), or low-dose buprenorphine under supervision. If you’re in severe pain and opioids are unavoidable, make sure your care team has cyproheptadine on hand and knows how to treat serotonin syndrome.
The Future Is Better-But Not Safe Yet
There’s progress. In 2023, the FDA approved a digital tool called SerotoninSafe that integrates with hospital systems and blocks dangerous prescriptions in real time. At Johns Hopkins, it cut prescribing errors by 76%. EHR systems like Epic now block these combos by default.
But problems remain. Community pharmacies still make errors at a 5.8% rate. Emergency rooms don’t always have the right info. And 31% of ER doctors still don’t know tramadol is dangerous with MAOIs.
Pharmaceutical companies are being held accountable. Purdue Pharma paid $4.7 million in 2021 for failing to warn about tapentadol interactions. The European Medicines Agency now requires mandatory training for all prescribers.
Still, over 1.2 million Americans are on MAOIs. And every one of them is at risk. Until every doctor, pharmacist, and patient knows the danger, this won’t end.
What If You’ve Already Taken Them Together?
If you’ve taken an opioid while on an MAOI-even once-and feel even slightly off, get help immediately. Don’t wait. Don’t assume it’s "just anxiety" or "a bad reaction."
Call 911 or go to the ER. Tell them: "I’m on an MAOI and took [name of opioid]. I think I might have serotonin syndrome."
Time is critical. The sooner you get treatment, the better your chance of survival. Delaying by even an hour can mean the difference between recovery and death.
Can I take Tylenol or ibuprofen with an MAOI?
Yes. Acetaminophen (Tylenol) and nonsteroidal anti-inflammatory drugs like ibuprofen (Advil) or naproxen (Aleve) are safe to use with MAOIs. They don’t affect serotonin or norepinephrine levels. These are the preferred pain relievers for anyone on an MAOI. Avoid opioids entirely unless under strict medical supervision with a known safe option like low-dose buprenorphine.
Is tramadol really that dangerous with MAOIs?
Yes. Tramadol is one of the most common causes of fatal serotonin syndrome in people on MAOIs. Despite being marketed as a "non-narcotic," it’s an opioid that strongly inhibits serotonin reuptake. Over 68 documented cases of serotonin syndrome have been linked to this combination since 2010. It’s not a matter of "maybe"-it’s a guaranteed risk. Never take tramadol with an MAOI.
How long does it take for an MAOI to leave your system?
The drug itself clears in days, but the enzyme inhibition is permanent. Your body needs to make new monoamine oxidase enzymes, which takes about 14 days. That’s why all medical guidelines require a 14-day washout period before starting any opioid with serotonergic activity. Even if you feel fine, the enzyme is still blocked. Don’t rush this timeline.
Can I use a fentanyl patch with an MAOI?
No. Fentanyl isn’t primarily serotonergic, but it triggers norepinephrine release. MAOIs prevent norepinephrine breakdown. This combo can cause a sudden, life-threatening spike in blood pressure. Even though it’s less likely to cause serotonin syndrome than tramadol, it’s still dangerous. Avoid all opioids unless specifically approved by a specialist familiar with MAOI interactions.
Are there any MAOIs that are safer than others?
The transdermal selegiline patch (Emsam) has lower brain penetration, meaning less interaction with central serotonin. But it still carries risk, especially at higher doses. Reversible MAOIs like moclobemide are less dangerous than irreversible ones, but still pose a threat with serotonergic opioids. No MAOI is completely safe with opioids. The safest approach is to avoid all opioids unless absolutely necessary and under expert care.
What should I do if my doctor prescribes an opioid while I’m on an MAOI?
Say no. Politely but firmly. Tell them you’re on an MAOI and that the combination can be fatal. Ask them to check the FDA’s black box warning and the American Psychiatric Association guidelines. If they insist, get a second opinion from a psychiatrist or pain specialist who specializes in complex drug interactions. Your life is not worth the risk.
So we're just supposed to trust the FDA now? Funny how they banned meperidine but still let tramadol slide under the radar. Classic regulatory capture. The real issue is doctors who think they're smarter than pharmacology textbooks.
Also why is everyone acting like this is new? I read about this in a 1980s neuropharmacology paper. We've known since the 60s.
This is so important-and I’m so glad someone finally put this out there in plain language! Please, if you’re on an MAOI, carry that warning card, tell every provider-even the dentist!-and don’t let anyone talk you out of it. Your life matters more than convenience. I’ve seen too many people dismissed because ‘it’s just a cough syrup’-and then it’s too late. You are not overreacting. You are surviving.
Y’all in the US are acting like this is some groundbreaking discovery. In Canada we’ve had mandatory MAOI interaction alerts since 2007. And in Europe? They train pharmacists to scream at you if you try to buy tramadol with an MAOI. Meanwhile, American docs still think ‘non-narcotic’ means ‘safe.’ LOL. You’re not special. You’re just behind.
Man I just had a friend in Toronto get prescribed tramadol after a root canal and she didn't even know her antidepressant was an MAOI... she ended up in the ER with a 105 fever and muscle spasms. Scared the crap out of her. Now she carries a laminated card in her wallet like a badge. Honestly? Everyone needs one. This isn't just medical advice-it's survival literacy.
i never knew this until i read this post. i thought tramadol was like tylenol with a kick. wow. i’m gonna check my meds right now. thank you for sharing this. i’m so glad i didn’t take it before. sometimes the scariest things are the ones you don’t even know are dangerous.
i think this is one of those things that gets buried because it’s not sexy like opioids and addiction. nobody talks about the antidepressant side of things. but this is literally a silent killer. we need more posts like this. not just for patients, but for med students too. i’m sharing this with my cousin who’s a nurse.
the real tragedy isn’t the interaction-it’s that we treat medicine like a menu. ‘I’ll take the serotonin boost, hold the dopamine, and add a side of norepinephrine.’ we’re not cooking a meal. we’re wiring a bomb. and someone’s always gonna forget the fuse.
MAOIs are outdated. Why are we still using them? If you need an antidepressant, take SSRIs. They’re safer, cheaper, and don’t turn you into a walking time bomb. Stop romanticizing the 60s psych drugs. This isn’t art. It’s pharmacology.
Buprenorphine’s the only one. Everything else? No. Just no.
I work in a rural ER. We had a case last month. Patient came in with rigidity, fever, no pulse ox reading. Turned out he took tramadol for back pain and didn’t think his ‘mood pill’ was an MAOI. He survived. But only because his wife recognized the symptoms from a YouTube video. That’s not healthcare. That’s luck.
I’ve been on selegiline patch for 3 years. I’ve had three surgeries. Every time, I hand the anesthesiologist a printed copy of this exact post. They always look at me like I’m crazy. Then they go silent. Then they call the pharmacy. That’s how you win. Be the annoying one. Be the one who reads the label.
this whole thing is just a giant waste of time. if you’re dumb enough to mix these drugs, you deserve what you get. just don’t be a burden on the system. we got real problems to deal with.