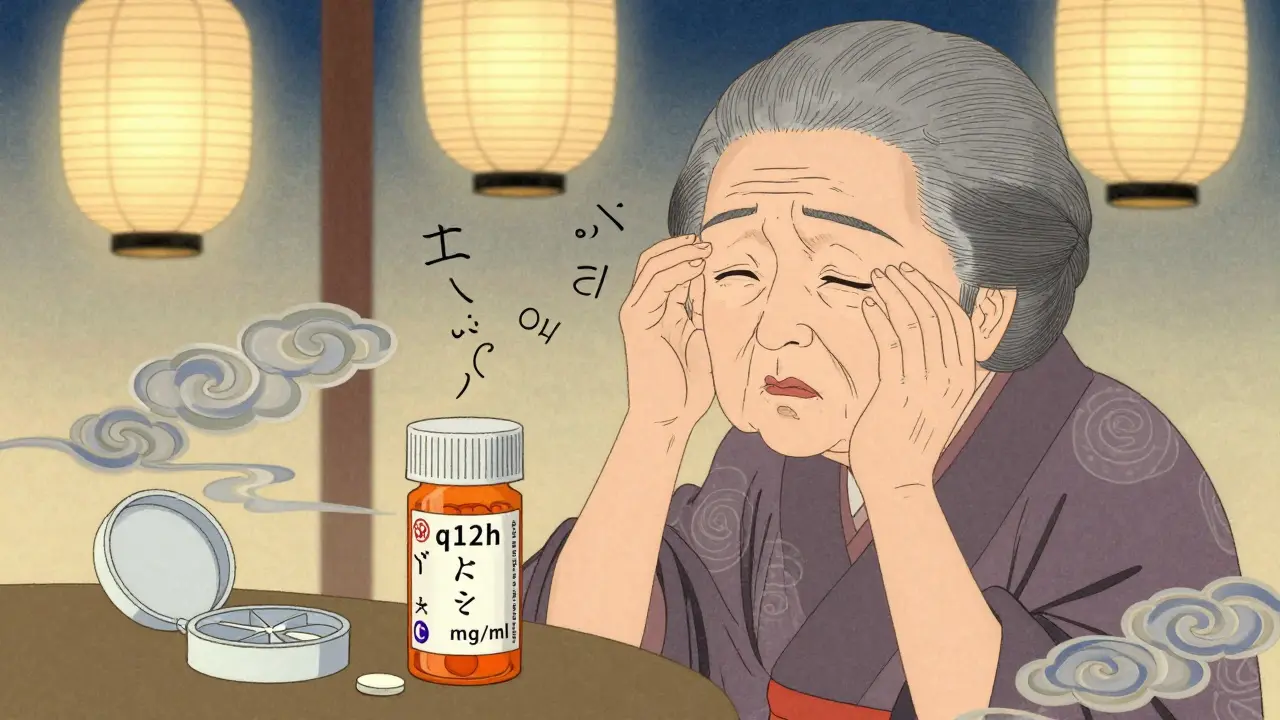
Every year, over 1.3 million medication errors happen in the U.S. - not because people are careless, but because the instructions on their pills don’t make sense. You might think reading "take one tablet twice daily" is simple. But for millions of people, that phrase is confusing, misleading, or even dangerous. If you’ve ever stared at a prescription bottle wondering when exactly to take your medicine, you’re not alone. Health literacy isn’t about being smart or educated - it’s about whether the system speaks your language. And right now, too many systems are failing.
Why Medication Labels Don’t Work for Most People
Standard medication labels are written like legal documents. Phrases like "q12h" or "take on an empty stomach" assume you know medical shorthand. But the average American reads at a 6th to 8th grade level. Meanwhile, most labels are written at a 10th to 12th grade level. That mismatch is deadly. A 2009 study found that 47% of patients misunderstood basic instructions like "take twice daily." They didn’t know if that meant morning and night, or every 12 hours. Others confused "mg" (milligrams) with "ml" (milliliters). One woman took albuterol from a plastic container she thought was a syringe - because the label didn’t say "for inhalation only." She ended up in the ER. Pediatric meds are even worse. A review of 200 top-selling children’s liquid medicines found that 63% used confusing charts with columns and ranges like "2-3 years: 5 mL." Parents didn’t know if that meant 5 mL total or 5 mL per dose. One parent told researchers: "I thought 'give 5 mL twice daily' meant 5 mL total over two doses, not 5 mL each time." That’s not a mistake - that’s a design failure.What Works: The Four Proven Strategies
There are four evidence-backed ways to fix this - and they’re not expensive. They just require clear thinking. 1. Use the Universal Medication Schedule (UMS)Stop saying "twice daily" or "every 8 hours." Instead, use four simple times: morning, noon, evening, bedtime. That’s it. A 2022 study in Wisconsin showed that when pharmacies switched to UMS labels, dosing confusion dropped by 47% among elderly patients taking five or more medications. One 72-year-old woman said: "I finally understood when to take my pills after they switched to morning/noon/evening/bedtime labels." No math. No guesswork. Just four times a day. 2. Write at a 5th-grade reading level
The Institute for Safe Medication Practices says all instructions should be written at or below a 5th-grade level. That means short sentences, active voice, no jargon. Instead of "Administer 10 mL orally every 6 hours as needed for pain," say: "Give 10 milliliters by mouth every 6 hours if pain is present." Merck’s team cut average sentence length from 15 words to 8.2. Comprehension jumped to 92% across all literacy levels. 3. Add pictograms
Pictures aren’t just for kids. A 2023 study showed that adding simple icons - like a sun for morning, a moon for bedtime, or a fork for "with food" - increased correct understanding by 28% among patients with low health literacy. The U.S. Pharmacopeia now requires these pictograms on all new prescription labels by May 2025. You’ll see a clock next to "morning," a spoon next to "take with food." No reading needed. 4. Use the teach-back method
Don’t just hand someone a bottle and say "do this." Ask them to explain it back. "Can you tell me how you’ll take this pill?" If they say, "I’ll take two when I feel bad," you know they didn’t get it. A 2022 UW Health study found that using teach-back reduced misunderstandings by 33%. It takes 1-2 minutes per medication. But it prevents hospital visits.
What Doesn’t Work - And Why
Some "solutions" look good on paper but fail in real life. Patient-centered labels (with clearer wording) reduced the chance of taking too much in 24 hours by 32%. But they didn’t stop people from taking pills too early, too often, or mixing them up. Why? Because people still didn’t understand "every 12 hours" vs. "twice daily." They thought they meant the same thing. Pharmacies that only changed font size or added bold text saw no improvement. Complexity isn’t fixed by making things bigger - it’s fixed by making them simpler. And don’t rely on apps or QR codes. Many older adults don’t use smartphones. Rural patients may not have good internet. If the answer isn’t on the bottle, it’s not accessible.Who’s Leading the Change?
Big hospitals are starting to get it. The CDC, FDA, and U.S. Pharmacopeia all now require health-literate labeling. By 2025, every prescription label in the U.S. must follow new design rules: pictograms, clear timing, fifth-grade language, one-column layout. Wisconsin Health Literacy’s toolkit has been used in over 150 clinics. They trained every pharmacist, nurse, and doctor to use UMS and teach-back. Within six months, medication-related readmissions dropped 22%. Malpractice claims fell 15%. Even small pharmacies are catching on. The American Society of Health-System Pharmacists found that 68% of large health systems now use health-literate labeling. Only 29% of small community pharmacies do. But that’s changing - because CMS now penalizes hospitals with high readmission rates. If your patient comes back because they took the wrong dose, you lose money.What You Can Do Right Now
You don’t need a hospital system to make this better. Here’s what you can do today:- Ask your pharmacist: "Can you write down when I should take this?"
- Use a pill organizer with morning, noon, evening, bedtime slots.
- Take a photo of your pill bottle and show it to a family member. Ask: "Does this make sense?"
- If you’re unsure about "every 12 hours" vs. "twice daily," ask: "Does that mean 8 a.m. and 8 p.m.?"
- Never guess. If you don’t understand, call your doctor or pharmacist. No question is too small.
The Bigger Picture
This isn’t just about pills. It’s about dignity. It’s about trust. When you can’t read your own medicine label, you feel powerless. You start to doubt yourself. You stop asking questions. You take the risk. But when the system speaks clearly, people take their medicine correctly. They stay out of the hospital. They live longer. And it costs less. Every $1 spent on clear labeling saves $3.75 in avoided care. The technology exists. The research is solid. The regulations are coming. The only thing missing is consistency. Your life depends on what’s written on that bottle. It shouldn’t be a guessing game.What does "take twice daily" really mean?
"Take twice daily" means two doses in one day - usually morning and evening. But many people think it means every 12 hours, or even that they can take both doses at once. To avoid confusion, ask your pharmacist: "Should I take it at 8 a.m. and 8 p.m.?" or "Can you write it as morning and bedtime?" The Universal Medication Schedule (UMS) recommends using "morning, noon, evening, bedtime" instead of medical terms like "twice daily."
Is "take with food" the same as "take after eating"?
No. "Take with food" usually means during the meal - not before or right after. But many people aren’t sure. Some take it 30 minutes before eating. Others wait an hour after. This matters for how well the medicine works or if it causes stomach upset. If you’re unsure, ask your pharmacist to show you a pictogram - like a plate with food - or write it as "take during your meal."
Why do some pills have "mg" and others have "mL"?
"mg" stands for milligrams - that’s the amount of active drug in a pill. "mL" stands for milliliters - that’s the volume of liquid medicine. Mixing them up can be dangerous. For example, taking 10 mg when you meant 10 mL could mean taking 10 times too much. Always check the unit. Liquid medicines come with a measuring cup - never use a kitchen spoon. If the label says "10 mg/5 mL," that means every 5 milliliters contains 10 milligrams of medicine.
Can I trust the dosing instructions on over-the-counter medicine?
Not always. A 2012 study found that 18.5% of top-selling children’s liquid medicines didn’t list the active ingredient on the front. Many used confusing charts instead of clear numbers. Always check the active ingredient - if you’re taking more than one medicine, you might accidentally double up. For example, Tylenol and many cold medicines both contain acetaminophen. Taking both can cause liver damage. Always read the "Active Ingredients" section - even if it’s small print.
What should I do if I still don’t understand my medicine label?
Call your pharmacist. They’re trained to explain this stuff. Ask them to write it down in simple words. Or ask for a visual aid - like a picture of a clock showing morning and night. If you’re helping an older relative, sit with them and go through each pill. Use the teach-back method: "Can you tell me how you’ll take this?" If they get it wrong, don’t assume they’re being stubborn - assume the label didn’t help. You’re not alone. Over half of adults struggle with medication labels. The problem isn’t you - it’s the system.
lol so now we need pictograms for pills? next they'll be drawing a little sun on the bottle so we know when to take it. i'm just gonna keep ignoring the label and guessing like i always have.
i had no idea so many people get confused by 'twice daily'... i always just took mine at breakfast and bedtime. but now i'm wondering if my grandma took hers wrong all these years 😅
I’ve seen this first-hand: my dad, 78, took his blood pressure med at 3 a.m. because he thought 'every 12 hours' meant 'whenever you wake up.' He ended up in the ER. The UMS system? Life-changing. My pharmacist now writes it out in crayon-like block letters. He doesn't need glasses to read it.
I’ve been using a pill organizer with morning/noon/evening/bedtime slots for a year now. It’s dumb simple, but it works. No more guessing. I even color-coded the pills with sharpies. My cat thinks I’m weird. I don’t care.
I work in a clinic and I’ve watched people cry because they felt stupid for not understanding their meds. This isn’t about intelligence - it’s about design. If we can make a microwave that doesn’t need a manual, we can make a pill bottle that doesn’t need a PhD to read. 🙏❤️
This is why Canada’s system is better. We don’t have these messes. In Quebec, labels are written in plain French, pictograms are mandatory, and pharmacists actually talk to you. Here? You get a slip of paper with Latin abbreviations and a 12-page warning leaflet. It’s a joke. America’s healthcare is a circus.
Let’s be real - the entire pharmaceutical-industrial complex is designed to obfuscate. Why? Because if you understood your medication, you might question why you need it in the first place. The system thrives on ambiguity. Pictograms? Teach-back? These are band-aids on a hemorrhage. The real issue is profit-driven medicine disguised as care. The label is the least of our problems.
I used to be one of those people who just shrugged and took it 'when I remembered.' Then my sister had a stroke from mixing OTC meds. Now I sit with my mom every Sunday and go through her pills with a checklist. We even make a little ritual out of it - tea, quiet music, and no judgment. It’s not just about safety - it’s about connection.
i just took my meds at 3am last night bc i was up scrolling and thought 'eh why not' 🤷♂️😂 also why do they even use mg and ml?? why not just say 'one spoon' or 'two dots'? i don't care about science i just wanna not die
I got my prescription yesterday. The label said 'take with food.' I ate a bag of chips. I’m fine. The system didn’t break. Maybe we’re overthinking this? People have been taking pills for 100 years without pictograms. Maybe the real problem is anxiety, not labels?
This whole thing is pathetic. You mean to tell me we need a whole movement because people can’t read? It’s not the label’s fault - it’s yours. If you can’t understand 'twice daily,' maybe you shouldn’t be managing your own meds. Someone else should do it. This isn’t empowerment - it’s enabling. The system isn’t broken. You are.
The adoption of health-literate labeling is a necessary evolution in public health infrastructure. The empirical data supporting the Universal Medication Schedule and pictographic communication is robust and reproducible across demographic strata. It is imperative that regulatory bodies enforce standardization, as inconsistent implementation undermines the integrity of therapeutic adherence protocols. The cost-benefit analysis is unequivocal.