
Getting prescription drugs shouldn’t mean choosing between food and insulin. But for millions of Americans, that’s the reality-until they find help through state and federal medication assistance programs. In 2025, these programs are more important than ever. Drug prices keep climbing, especially for insulin, specialty meds, and chronic condition treatments. While Medicare Part D covers a lot, it doesn’t cover everything-and the out-of-pocket costs can still crush a fixed income. That’s where state programs step in. But here’s the catch: what you get depends entirely on where you live.
How State Medication Programs Work (And Why They’re So Different)
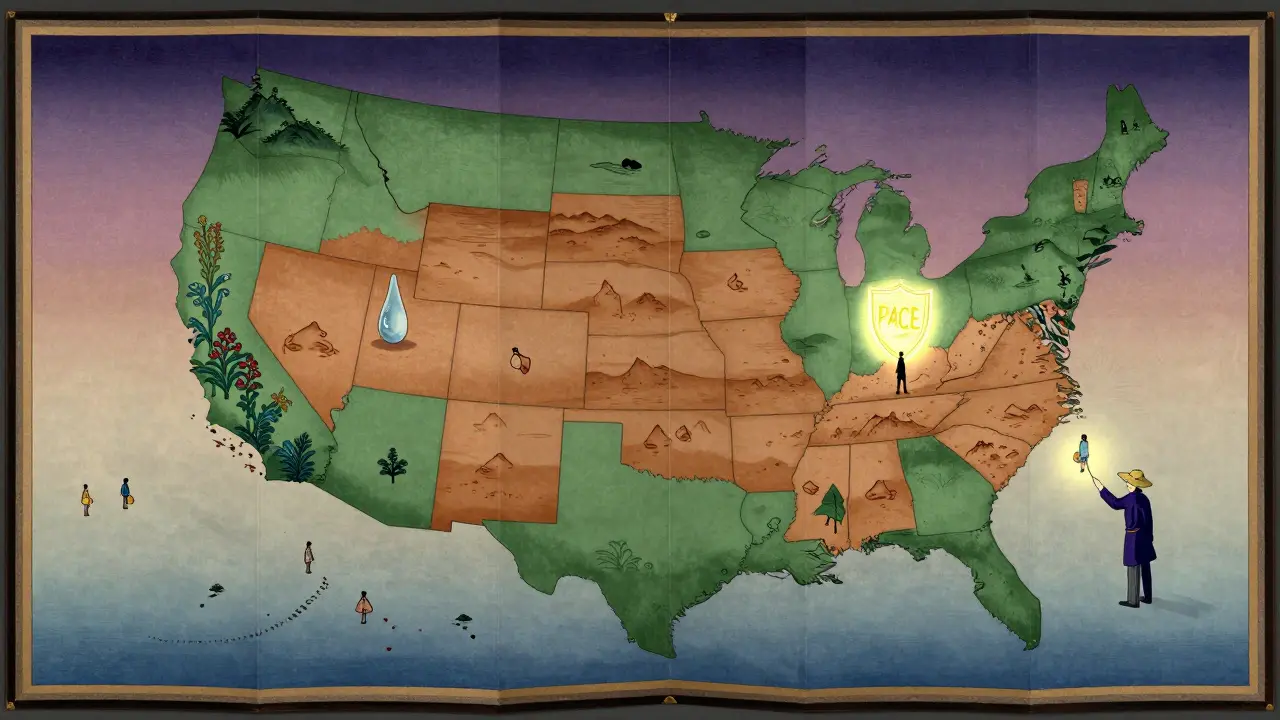
Every state runs its own version of a Pharmaceutical Assistance Program (SPAP), but there’s no national standard. Some are simple copay helpers. Others cover full premiums. A few even pay for drugs Medicare won’t touch. The biggest difference? Eligibility. Some states only help seniors over 65. Others include disabled adults under 65. A few even cover low-income families.
Take New Jersey’s PAAD program. It’s been around since 1967 and helps people with incomes under $27,470 (individual) or $36,900 (couple). You pay just $5 for generics and $7 for brand-name drugs. PAAD even pays your Medicare Part D premium if it’s under $34.70/month. But if you live in Wyoming? There’s a SPAP-but it only has $15 million to spread across the whole state. That means fewer people qualify, and coverage is much tighter.
That’s the problem with state programs: they’re patchwork. If you move from Pennsylvania to Florida, your help might vanish-or change completely. A 2024 study by the Medicare Rights Center found that 63% of people who moved between states faced gaps in coverage. One woman in Ohio lost her insulin coverage for six weeks after relocating to Georgia. She paid $1,200 out of pocket before finding a new program.
Medicare Extra Help: The Federal Backup
If you’re on Medicare and have limited income, you might qualify for Extra Help-the federal program that cuts your Part D costs to near zero. In 2025, if you earn less than $23,475 a year (or $31,725 as a couple) and have less than $17,600 in resources (savings, investments, property beyond your home), you’re eligible.
What does that mean in real dollars? You pay $0 for premiums and deductibles. Generics cost $4.90 per prescription. Brand-name drugs? $12.15. That’s cheaper than most state programs. And starting in 2025, your total out-of-pocket drug spending is capped at $2,000 a year. Before, it was $7,050. That’s a massive win.
But here’s the catch: Extra Help has strict rules. Your bank account, 401(k), and even the value of your second car count toward the $17,600 limit. In California or New York, where rent and groceries cost more, that limit doesn’t stretch far. A 2025 KFF analysis found that many people who clearly need help are turned away because their savings are $2,000 over the cap-money they saved for emergencies, not luxury.
State Programs That Go Beyond Medicare
Some states don’t just fill gaps-they expand coverage. California’s Medi-Cal Rx program adds 127 specialty drugs to its formulary that Medicare Part D won’t cover. That includes treatments for rare autoimmune diseases, certain cancer drugs, and advanced diabetes therapies. If you’re on Medicare and live in California, you can get both Extra Help and Medi-Cal Rx. You pay nothing for those extra meds.
Pennsylvania’s PACE program does something similar. It covers drugs not on Medicare’s list and pays your Part D premium. But here’s the twist: you have to apply for Extra Help first. Only after that does PACE kick in. The process takes 120 days on average. People waiting for approval often go without meds. One man in Pittsburgh paid $872 for a heart medication during his 3-month wait. He didn’t know he could get emergency aid from his local SHIP counselor.
That’s where the State Health Insurance Assistance Program (SHIP) comes in. Every state has free, local SHIP counselors-14,000 of them nationwide. They help you fill out forms, compare programs, and even appeal denials. In 2024, they handled 4.2 million requests. Yet, 42% of eligible people never apply. Why? The paperwork is overwhelming. The average applicant spends 8.5 hours filling out forms. That’s a full workday.
What’s Changing in 2025 (And What’s Coming)
Big changes are happening. Starting in 2025, people on Medicaid or Extra Help can switch their Medicare drug plan once a month-not just once a year. That’s huge. If your drug gets pulled from the formulary, you can move to a better plan fast.
The $2,000 out-of-pocket cap for Part D is another game-changer. Before, people hit the “catastrophic” phase after spending $7,050. Now, you’re protected after $2,000. That means seniors on expensive meds like Ozempic or Humira won’t be bankrupted.
But not everything is improving. Drug prices are still rising-specialty meds up 12.3% a year. Meanwhile, state SPAP budgets are growing only 4-6%. Seven states are projected to run out of money by 2026. Some are already cutting coverage. Eighteen states have tightened prior authorization rules or removed drugs from their lists. That means even if you qualify, your meds might not be covered anymore.
Looking ahead, 12 more states plan to expand SPAPs by 2027. California, Texas, and Florida are leading the way. But until there’s a national standard, you’ll still be playing a guessing game if you move.
How to Apply (And What to Do If You’re Denied)
Applying for Extra Help? Fill out Form SSA-1020 online at ssa.gov or call 1-800-772-1213. You’ll need your Social Security number, proof of income (tax returns or pay stubs), and asset info (bank statements, investment accounts). Processing takes 90 days on average. If you’re denied, you can appeal-but you’ll need to act fast.
For state programs, you’ll need to find your state’s SPAP website. New Jersey’s PAAD? Go to nj.gov/paad. Pennsylvania’s PACE? Visit aging.pa.gov. Most states have online portals now. But don’t wait until you’re out of meds. Start early. Applications can take 30 to 90 days.
If you’re denied, don’t give up. Call your local SHIP counselor. They’ve seen every excuse the system uses. They know which documents get rejected and how to fix them. They’ve helped people get approved after three failed attempts. And they’re free.
Who Gets Left Behind?
Not everyone qualifies. If you make $25,000 a year but have $20,000 in savings, you’re ineligible for Extra Help-even if you’re struggling to afford your prescriptions. If you’re 58 with a chronic illness and don’t qualify for Medicare yet, state programs might not cover you. If you’re a veteran, you might be better off using VA benefits instead.
And then there’s the hidden group: people who don’t know they qualify. A 2024 KFF survey found that 28% of Medicare beneficiaries with drug coverage still couldn’t afford their meds. But 41% of those people weren’t even enrolled in any assistance program. They didn’t know it existed. Or they thought the process was too hard.
One Reddit user from New Jersey wrote: “PAAD saved me over $400 a month on my diabetes meds. I didn’t apply for a year because I thought I made too much. Turns out, I qualified.”
Don’t assume you’re too rich. Don’t assume you’re too young. Don’t assume it’s too complicated. Check it. Even if you think you don’t qualify, you might.
What You Can Do Right Now
- Go to medicare.gov and use the “Extra Help” eligibility tool. It takes 5 minutes.
- Find your state’s SPAP website. Search “[Your State] pharmaceutical assistance program.”
- Call 1-800-MEDICARE and ask for your local SHIP counselor. They’ll walk you through it.
- If you’re on insulin, check if your state has a separate insulin affordability program. Over 30 do.
- Don’t wait for a crisis. Apply before you run out of meds.
Prescription drug help isn’t perfect. It’s confusing. It’s uneven. But it’s real-and it works. People are saving $4,000 to $5,000 a year because they took the time to apply. You can too.
Who qualifies for Medicare Extra Help in 2025?
To qualify for Medicare Extra Help in 2025, you must have limited income and resources. For individuals, your annual income must be $23,475 or less, and your resources (savings, investments, property beyond your home) must be $17,600 or less. For married couples living together, the income limit is $31,725 and the resource limit is $35,130. You automatically qualify if you receive Medicaid, Supplemental Security Income (SSI), or a Medicare Savings Program.
Do all states have medication assistance programs?
Yes, 32 states operate some form of State Pharmaceutical Assistance Program (SPAP) as of 2025. These programs vary widely-some help only seniors, others include disabled adults under 65. A few states like New Jersey and Pennsylvania offer robust coverage, while others like Wyoming have limited funding and strict eligibility. Not every state offers the same benefits, and some only cover certain drugs or populations.
Can I get help if I’m under 65 and disabled?
Yes, if you’re under 65 and receive Social Security Disability Insurance (SSDI) or are eligible for Medicare due to disability, you may qualify for Medicare Extra Help. Many state SPAPs also cover disabled adults under 65 with low income. For example, New Jersey’s PAAD program includes disabled individuals regardless of age if they meet income and residency requirements. Always check your state’s specific program rules.
What if my medication isn’t covered by my state’s program?
If your drug isn’t on your state’s formulary, you can request an exception or appeal. Most SPAPs have an appeals process, though it can take 6-8 weeks. Meanwhile, contact your local SHIP counselor-they can help you find alternative drugs covered by your program or connect you with patient assistance programs from drug manufacturers. Some states, like California, cover additional specialty drugs not included in Medicare Part D, so check if your state offers broader coverage.
How long does it take to get approved for medication assistance?
Medicare Extra Help applications take about 90 days to process. State programs vary: New Jersey’s PAAD averages 30 days, while Pennsylvania’s PACE can take up to 120 days because it requires Extra Help approval first. If you’re facing a medical emergency, ask your SHIP counselor about emergency aid or temporary assistance from drug manufacturers. Some pharmacies offer 30-day free samples while you wait.
Can I apply for both state and federal help at the same time?
Yes, and you should. Many people qualify for both Medicare Extra Help and their state’s SPAP. In states like Pennsylvania, you must apply for Extra Help first, then PACE covers what’s left. In New Jersey, PAAD pays your Part D premium and reduces your copays. In California, Medi-Cal Rx adds drugs Medicare doesn’t cover. Applying for both can cut your drug costs by 70% or more. Always check if programs stack-most do.
What should I do if I’m denied assistance?
Don’t accept a denial as final. First, review your application for missing documents-like bank statements or tax forms. Then, contact your local State Health Insurance Assistance Program (SHIP) counselor. They’ve helped thousands appeal denials. You can also request a formal appeal from the agency that denied you. Many people get approved on their second try after fixing small errors. If you’re in urgent need, ask about emergency drug programs from pharmaceutical companies or nonprofit organizations like NeedyMeds.
Next Steps: Don’t Wait Until It’s Too Late
If you’re paying more than $100 a month for prescriptions, you’re not alone-and you’re not helpless. The system is broken, but the help is there. You just have to ask. Start with Extra Help. Then check your state’s program. Talk to a SHIP counselor. Even if you think you make too much, you might not. The rules are confusing, but the savings are real. People are saving thousands. You can too.
Let’s be real-this whole system is a joke. You’re telling me a 62-year-old with $18,000 in savings can’t get insulin because they once bought a used Honda? Meanwhile, billionaires get tax breaks for yachts. This isn’t healthcare policy-it’s a cruel lottery where your zip code determines whether you live or die. And don’t even get me started on how ‘extra help’ excludes people who’ve saved responsibly. The system doesn’t fail the poor-it punishes the prudent.
Also, SHIP counselors? Cute. They’re overworked, underfunded, and probably using clipboards from 1998. If you think filling out 8.5 hours of paperwork is ‘accessible,’ you’ve never had to do it while managing three chronic conditions and a part-time job.
And yes, I’ve applied. Twice. Got denied both times because my ‘investment account’ had $2,100 in Vanguard. That’s not wealth. That’s my funeral fund.
Someone needs to burn this whole thing down and start over.
Actually, you’re all missing the point. The real problem isn’t the programs-it’s that people are too lazy to just get a second job. I worked two shifts at Walmart while on dialysis. I paid for my meds. You think the government owes you free drugs? No. You owe it to yourself to hustle.
Also, ‘insulin affordability programs’? Please. Insulin costs $30 a vial in Canada. Why not just move? The system’s not broken-it’s just not designed for whiners.
Hey, I just want to say-this post is incredibly helpful. I’m a retired nurse and I’ve helped dozens of patients navigate these programs. One thing no one mentions: if you’re denied Extra Help, ask for a ‘reconsideration’ and submit a letter from your doctor explaining your medical necessity. It’s not guaranteed, but it works way more often than people think.
Also, don’t overlook manufacturer coupons. Even if you’re denied state aid, companies like Novo Nordisk and Eli Lilly have free drug programs for people under 400% of the poverty line. I’ve seen people go from $600/month to $0 with just a 10-minute call.
And yes, the paperwork sucks. But you don’t have to do it alone. Call 1-800-MEDICARE and ask for your SHIP counselor by name. They’re not robots-they’re people who’ve been doing this for 20 years. They’ll fix your typos, reformat your forms, and even call the state for you.
One woman I helped got approved after three denials. She cried when she got the letter. Don’t give up. You’re not alone.
Oh, so now we’re pretending this is a moral crisis? Let’s analyze the structural incentives. SPAPs exist because federal policy is intentionally fragmented-designed to create regulatory arbitrage for pharma. The $2,000 cap? A political stunt to appease seniors before the next election. Meanwhile, drug companies raised prices 12.3% because they knew Congress would cave.
And the ‘SHIP counselors’? A Band-Aid on a hemorrhage. 14,000 of them can’t fix a system where Medicaid expansion was politicized into a patchwork quilt of neglect. You’re not helping people-you’re enabling a broken architecture.
Also, ‘apply early’? That’s not advice. That’s victim-blaming. If your meds are expiring in 3 days and the state takes 90 days to process, you’re not ‘unprepared’-you’re a casualty of neoliberal governance.
Real solution? Single-payer. Everything else is rearranging deck chairs on the Titanic.
Thank you so much for sharing this!! 😊 I just applied for PAAD last week and I’m so nervous!! I’m 59 and on SSDI and I was terrified I wouldn’t qualify because I have a little in savings… but now I feel hopeful!! I called my SHIP counselor and she said my $19,000 is fine because it’s from my late husband’s life insurance!! 🥹 I’m so glad I didn’t give up!!
Also, I didn’t know about the insulin programs!! I’m going to check that right now!! Thank you thank you thank you!! 💕
Why are we even talking about this? Canada has universal healthcare. Why are Americans still pretending this is normal? You people pay more for insulin than Germans pay for heart surgery. This isn’t ‘help’-it’s shame. You should be ashamed. Fix your system or just admit you don’t care about your elderly.
Also, ‘apply early’? LOL. You think people in rural Ohio have time to fill out 8 hours of paperwork? They’re working 60-hour weeks just to afford rent. Stop blaming the victims.
Send the money. End the nonsense.
As someone from India, I’m stunned by how complex this is. In my country, the government provides free insulin to all diabetics through public clinics-even for undocumented migrants. I understand the U.S. has a different economic model, but the moral cost here is staggering.
What baffles me is that this isn’t about money-it’s about prioritization. The U.S. spends more on healthcare per capita than any nation on Earth. Yet people are choosing between insulin and groceries.
I don’t know your system well, but I do know this: if a society lets its most vulnerable die because of bureaucratic red tape, it has lost its soul. I hope you find a way to fix this.
Okay, I need to say this because I’ve been there. My mom was on $1,200/month for her cancer meds. She cried every night because she was skipping doses to make it last. We applied for Extra Help. Got denied. We appealed. Got denied again. We were ready to sell her wedding ring.
Then we found SHIP. One counselor-her name was Linda-sat with us for 3 hours. She found a loophole: my mom’s 401(k) wasn’t counted because it was in payout mode. We resubmitted. Approved. Her copay dropped to $4.75.
I’m not saying it’s fair. I’m saying it’s possible. Don’t listen to the cynics. Don’t believe the ‘it’s too hard’ lie. Someone out there has walked this path. Call SHIP. Now. Don’t wait. Please.
I’m still crying typing this. If you’re reading this and you’re scared-take a breath. You’ve got this.
Just saw Aliza’s comment-and I want to add something she didn’t mention: if you’re denied because of your 401(k), ask if your plan qualifies as a ‘retirement account under IRS Section 401(a)’. Some states don’t count those at all, but the forms don’t explain that. SHIP counselors know this trick. It’s not a loophole-it’s a rule that got buried in the paperwork.
Also, if you’re on SSDI and under 65, you’re eligible for Extra Help even if you’re not on Medicare yet. That’s a common mistake. Call 1-800-MEDICARE and say, ‘I’m on SSDI and need help applying for Extra Help.’ They’ll connect you.
And one more thing-some states offer retroactive coverage. If you paid out of pocket while waiting, you can get reimbursed. Don’t assume you’re out of luck. Ask. Always ask.