More than 1 in 5 people worldwide have a fungal skin infection at any given time. It’s not rare. It’s not unusual. It’s not something you caught because you were careless. Fungal skin infections like Candida and ringworm are common, often misunderstood, and sometimes misdiagnosed - even by doctors. If you’ve had a stubborn red patch that won’t go away, or a itchy, peeling foot that keeps coming back, you’re not alone.
What Exactly Is Ringworm?
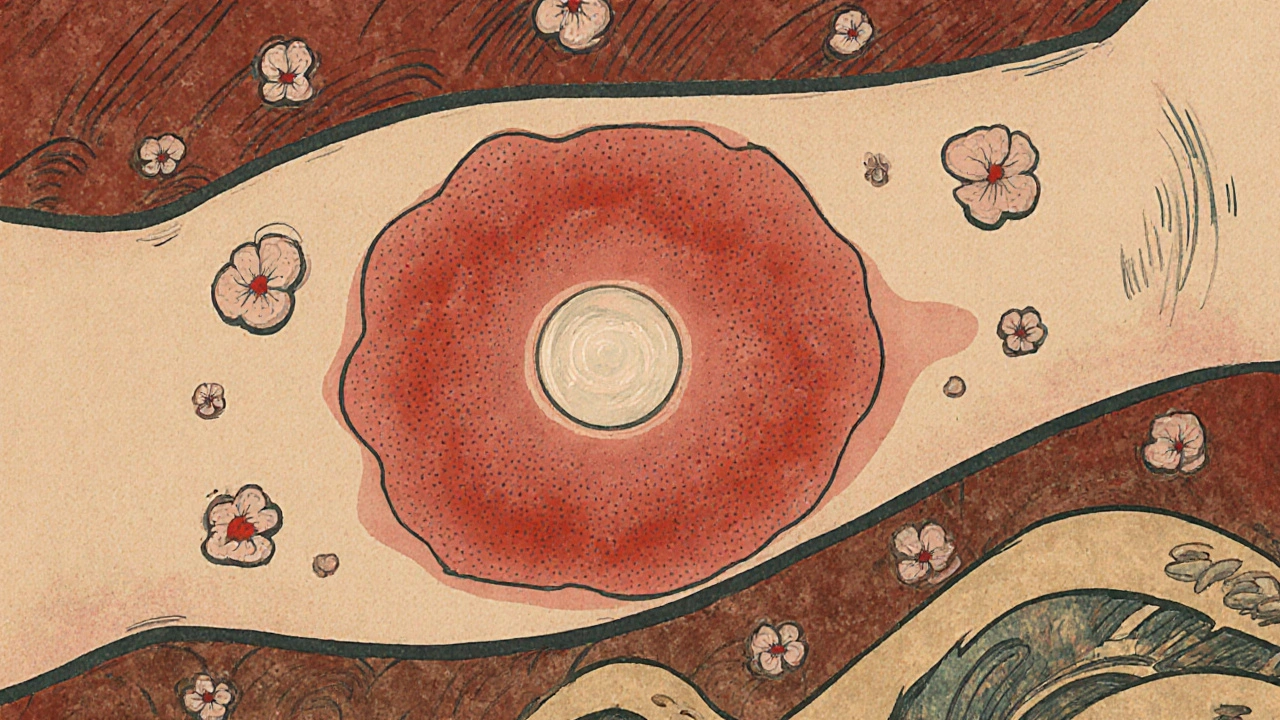
Ringworm isn’t caused by a worm. The name comes from the old belief that the circular, raised rash looked like a worm under the skin. In reality, it’s a fungal infection called tinea, caused by fungi that feed on keratin - the protein in your skin, hair, and nails. The most common culprits are fungi from the Trichophyton genus, responsible for 80-90% of cases.
Ringworm shows up differently depending on where it lives. On the body (tinea corporis), it’s a red, scaly ring with a raised edge and clearer center. On the feet (tinea pedis), it’s peeling, cracked skin between the toes - often called athlete’s foot. On the scalp (tinea capitis), it can cause patchy hair loss in kids. And on the nails (tinea unguium), it thickens, yellows, and crumbles the nail.
It spreads easily. Kids pick it up from pets - especially cats and dogs. Adults get it from shared showers, gym mats, or sweaty socks. In fact, 15-25% of adults globally have athlete’s foot, and that number jumps to 50% in military settings. The good news? Most cases respond well to treatment. The bad news? Many people stop using their cream too soon, and the infection comes back.
Candida: The Yeast That Turns Against You
If ringworm is the mold that lives on dead skin, Candida is the yeast that lives inside you - and sometimes overgrows. Candida albicans is the usual offender, normally harmless in small amounts in your mouth, gut, or vagina. But when conditions get warm and wet - like under your breasts, in your groin, or under a diaper - it multiplies fast.
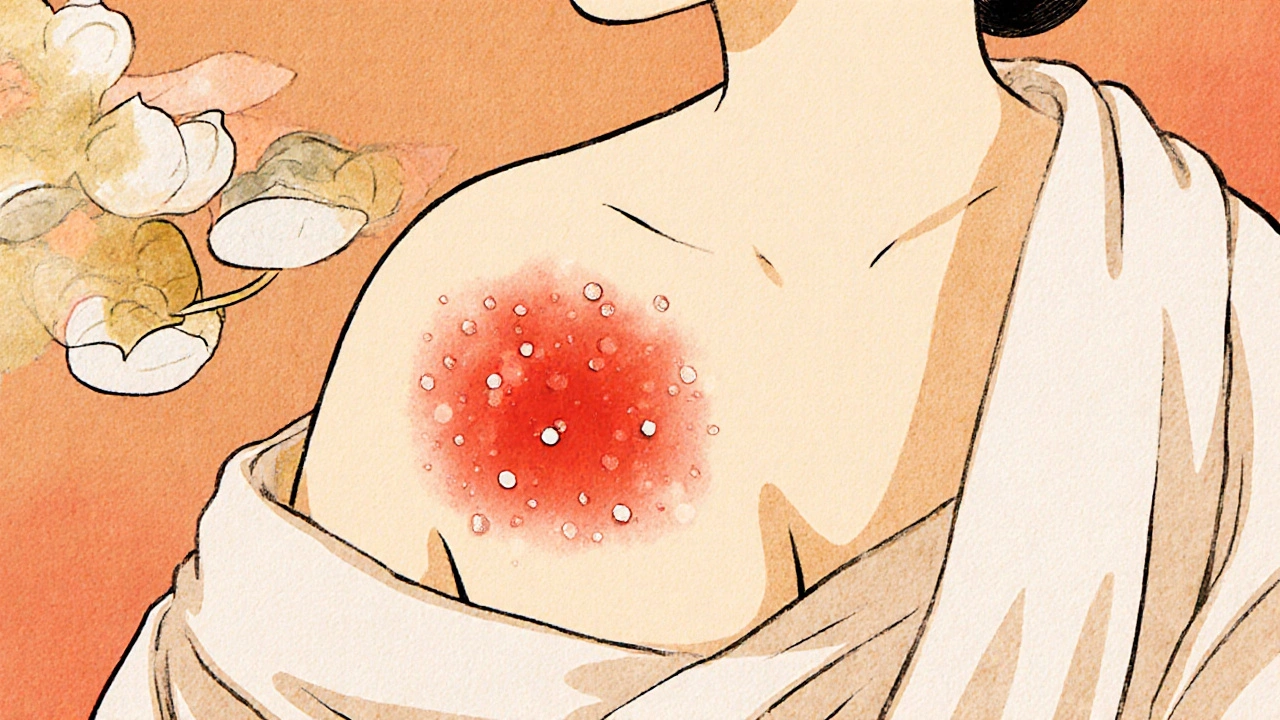
Candida infections look different from ringworm. Instead of a ring, you get a bright red, moist, sometimes shiny patch. Look closely, and you might see tiny red bumps (satellite pustules) around the edges. In babies, it’s diaper rash that doesn’t improve with zinc oxide. In adults, it’s often between the thighs, under the breasts, or in skin folds. Vaginal yeast infections are also Candida - and they’re incredibly common, affecting 75% of women at least once.
What makes Candida tricky is that it’s not always from outside. Stress, antibiotics, diabetes, or a weakened immune system can trigger it from within. People with diabetes are 2.5 times more likely to get skin Candida. And in hospitals, a dangerous strain called Candida auris is spreading - it’s resistant to multiple drugs and can cling to skin for weeks.
How Do You Know Which One You Have?
Doctors don’t always get it right. Studies show primary care providers correctly identify ringworm only half the time. Many patients are told they have eczema or psoriasis - and get steroid creams that make the fungus worse.
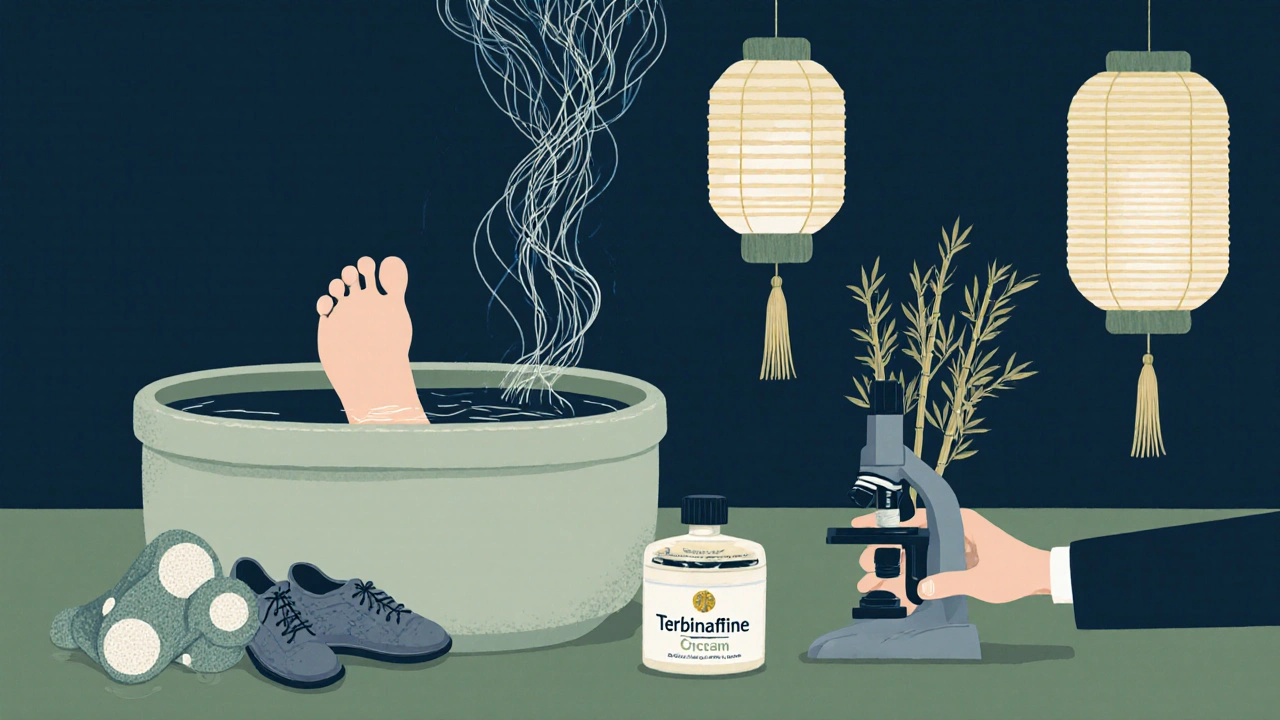
The quickest, cheapest way to check? A KOH test. A doctor scrapes a bit of skin, mixes it with potassium hydroxide, and looks under a microscope. Fungal threads show up like little strings. It’s fast, accurate in 70-80% of cases, and done right in the office.
Culture tests take weeks, but they’re used when the diagnosis is unclear or the infection keeps coming back. Newer DNA tests are popping up in labs, giving results in days instead of weeks. But for most cases - especially clear ringworm or classic Candida - doctors start treatment based on how it looks.
Topical Antifungals: What Actually Works
For mild cases, creams and sprays are the first line. Two main classes do the job: azoles and allylamines.
- Azoles (clotrimazole, miconazole): These stop the fungus from making its cell membrane. They’re in most over-the-counter creams. Good for Candida and mild ringworm. You need to use them for 2-4 weeks, even if it looks better after a few days.
- Allylamines (terbinafine, naftifine): These kill the fungus outright. Terbinafine (Lamisil) is often more effective for ringworm, especially on the body and feet. Studies show it clears tinea corporis in 70-90% of cases with just 1-2 weeks of use.
For Candida diaper rash in babies, nystatin cream works well. For vaginal yeast, clotrimazole suppositories are standard. For skin folds, keeping the area dry is just as important as the cream. Use a fan, wear loose cotton, and change out of sweaty clothes right away.
One big mistake? Using steroid creams. They reduce redness and itching - so people think it’s working. But steroids suppress the immune response, letting the fungus spread. If your rash gets worse after using hydrocortisone, stop. You might have a fungal infection.
Oral Antifungals: When Creams Aren’t Enough
Topical treatments fail for nail infections. That’s because the fungus hides under the nail, where cream can’t reach. For tinea unguium, you need pills.
Terbinafine (250mg daily) is the gold standard. It cures 80-90% of nail infections after 6-12 weeks. Fluconazole (150mg weekly) is another option, especially for Candida. But here’s the catch: terbinafine can affect your liver. Blood tests are needed before and during treatment. Fluconazole is safer for the liver but less effective for dermatophytes.
And resistance is growing. About 5-7% of Trichophyton rubrum - the most common ringworm fungus - is now less responsive to terbinafine in North America. That’s why doctors are starting to use shorter courses or combination therapy.
For stubborn Candida, especially recurrent vaginal infections, a new drug called ibrexafungerp (Brexafemme) was approved in 2023. It reduced recurrences by 50% in clinical trials - a big step forward.
Why Do These Infections Keep Coming Back?
Recurrence is the #1 complaint. In one survey of 1,200 people, 35% said their fungal infection came back within a year. Why?
- You stopped the cream too early. Fungus can hide under the skin even after the rash fades.
- You didn’t clean your shoes or socks. Fungus lives in damp fabric and leather.
- You didn’t treat the source. If your dog has ringworm, you’ll keep getting it back.
- Your skin stays moist. Tight clothes, sweating, not drying between toes - all feed the fungus.
People with diabetes, obesity, or weakened immune systems are more likely to have recurring infections. That’s why managing blood sugar, losing weight, and avoiding prolonged antibiotic use matters.
Some users on Reddit and health forums swear by probiotics - especially Lactobacillus - to prevent Candida from bouncing back. While not a replacement for antifungals, a small study of 850 people found that 65% had fewer recurrences when they took probiotics alongside their treatment. It’s not magic, but it might help.
What You Can Do Today
If you suspect a fungal infection:
- Don’t use steroid creams unless a doctor says so.
- Start with an OTC terbinafine cream for ringworm, or clotrimazole for Candida.
- Apply it beyond the edge of the rash - at least an inch past.
- Keep the area clean and dry. Use talc-free powder if needed.
- Wash your towels, sheets, and clothes in hot water.
- Don’t share shoes, socks, or towels.
- If it doesn’t improve in 2 weeks, see a doctor.
For nail infections or persistent rashes, don’t wait. Get a KOH test. Ask if oral treatment is needed. And if you’ve had this before, think about what triggered it - tight shoes? Antibiotics? Diabetes? Address the root cause, not just the rash.
The Bigger Picture
Fungal skin infections aren’t just a nuisance. They’re a growing public health issue. The global antifungal market hit $14.7 billion in 2022. Over-the-counter sales in the U.S. alone reached $1.8 billion. But resistance is rising. The WHO now lists Candida auris as a critical threat. By 2050, drug-resistant fungal infections could kill 1.6 million people a year if we don’t act.
That’s why research is accelerating. New drugs like olorofim are in trials. The NIH is funding $32 million for fungal microbiome studies. We’re learning that fungi don’t just cause disease - they’re part of our ecosystem. The goal isn’t to kill every fungus. It’s to restore balance.
For now, you don’t need to panic. Most fungal skin infections are easy to treat - if you know what you’re dealing with. Don’t guess. Don’t delay. Use the right treatment, finish the course, and protect yourself from reinfection. Your skin will thank you.
Oh wow, a whole essay on fungus? I’m so moved. Let me grab my tissue box - I’ve been crying over ringworm since childhood. Seriously though, if you think your doctor’s ‘probably eczema’ diagnosis is bad, try being a woman with recurring yeast infections who’s been told ‘it’s just stress’ for seven years. At least this post doesn’t call it a ‘lifestyle issue.’
Also, terbinafine? Cute. Try getting a prescription in Lagos without being asked if you’re ‘trying to lighten your skin.’
I had this for months. Between my thighs. Red. Itchy. No one would believe me. I went to three doctors. One said it was ‘allergies.’ Another said ‘wear cotton.’ I cried in the bathroom after the third visit. Then I found clotrimazole on Amazon. Two weeks. Gone. No one talks about how lonely this is.
Also, my mom used to rub coconut oil on it. It helped. Not cure. But helped.
Let me tell you something - this isn’t just about skin. This is about the quiet, invisible war your body fights every single day while you’re scrolling TikTok and eating gluten-free crackers. Fungi? They’ve been around since dinosaurs pooped. And now? We’ve got this beautiful, terrifying, microscopic rebellion happening under our armpits and between our toes - and we treat it like a personal failure. I’ve seen grown men cry because their athlete’s foot came back after a weekend at the gym. I’ve seen women hide their legs in winter because of a rash that wasn’t eczema, wasn’t psoriasis, wasn’t ‘just dry skin’ - it was Candida, and it was screaming for help.
And yes, terbinafine works. But here’s the real magic? Drying your feet like your life depends on it. Because it does. Your feet are your foundation. If they’re rotting? You’re not walking - you’re limping through life. And if you’re using hydrocortisone like it’s chapstick? You’re basically handing the fungus a golden ticket to a five-star resort inside your epidermis. Stop. Just stop.
And if you think probiotics are ‘woo-woo’ - go read the 2022 meta-analysis from the Journal of Clinical Mycology. Lactobacillus doesn’t just ‘help.’ It reprograms your microbiome like a silent ninja. This isn’t alternative medicine. This is science with socks.
And for the love of all that’s holy - wash your towels. Not ‘sometimes.’ Not ‘when you remember.’ Every. Single. Time. Fungus doesn’t care if you’re ‘clean.’ It only cares if you’re damp.
OMG I HAD THIS SO BAD LIKE WHO EVEN CARES ABOUT TINEA??? I WAS LIKE ‘IT’S JUST A RASH’ AND THEN I STARTED USING STEROID CREAM AND OMG IT GOT WORSE LIKE I WAS A FREAKING MUSHROOM???
AND THEN I TRIED COCONUT OIL AND IT WAS LIKE A MIRACLE??? I MEAN LIKE I’M NOT EVEN KIDDING I WAS CRYING I WAS SO HAPPY???
AND WHY DO DOCTORS EVEN EXIST IF THEY CAN’T TELL THE DIFFERENCE BETWEEN ECZEMA AND A FUNGUS???
ALSO I’M FROM INDIA AND WE JUST USE HIMALAYAN NEEM SOAP AND CALL IT A DAY???
WHY IS EVERYONE SO DRAMATIC ABOUT THIS???
My cousin in Mumbai had this for years. No one helped him. He was ashamed. We thought it was just sweat. Then one day his sister saw it - she works in a pharmacy. She gave him terbinafine. One month. Gone.
People here think it’s ‘dirty’ - but it’s not about dirt. It’s about moisture. Heat. Stress. We forget that.
Also, washing clothes in hot water? Yes. But in India, many don’t have washing machines. So we soak in salt water. Works. Not perfect. But helps.
Don’t blame yourself. Fungus doesn’t care who you are. It just wants a warm place to live.
And please - don’t use steroid cream. I’ve seen what it does.
While the preceding exposition on dermatophytosis and candidiasis is broadly accurate, it lacks a rigorous contextualization within the broader framework of antimicrobial stewardship and the epidemiological trajectory of fungal resistance. The assertion that terbinafine exhibits efficacy in 70–90% of tinea corporis cases is supported by randomized controlled trials, notably those published in the British Journal of Dermatology (2018) and the Journal of the American Academy of Dermatology (2020). However, the increasing prevalence of resistance alleles in Trichophyton rubrum - particularly the CYP51A1 and MFS transporter mutations - necessitates a paradigm shift from empirical monotherapy to culture-guided, molecularly stratified treatment protocols.
Furthermore, the uncritical endorsement of over-the-counter antifungals without confirmatory diagnostic testing undermines public health initiatives. The KOH preparation, while expedient, possesses a sensitivity of only 70–80%; thus, reliance on clinical presentation alone risks misdiagnosis in atypical presentations, particularly in immunocompromised populations. The WHO’s designation of Candida auris as a critical pathogen is not hyperbolic - it is a sentinel event in global infectious disease surveillance.
Probiotic supplementation, while biologically plausible, remains adjunctive and lacks robust phase III validation for cutaneous candidiasis recurrence prevention. The cited 65% reduction statistic is derived from a single-center observational cohort, not a double-blind placebo-controlled trial. Until such evidence emerges, clinical recommendations must remain anchored in microbiological confirmation and evidence-based guidelines - not anecdotal Reddit testimonials.
Just wanted to add something practical: if you’ve had a recurring fungal infection, check your shower drain. Fungus thrives in the gunk that builds up over time. I had athlete’s foot come back for three years - until I scrubbed the drain with bleach and vinegar every week. No magic. Just hygiene.
Also, if you’re using a gym mat, bring your own towel. Even if it’s ‘clean.’ Fungus survives for weeks on surfaces. I’ve seen it.
And yes - terbinafine works. But only if you use it like a doctor told you to. Not ‘until it looks better.’ Until it’s GONE. Under the skin too.
This isn’t drama. It’s biology.
FUNGUS IS THE REAL VILLAIN OF OUR TIME, PEOPLE. I’M NOT KIDDING. IT’S THE SILENT, SLIMY, SWEATY SPOOK THAT LIVES IN YOUR SOCKS, YOUR SHOES, YOUR GYM BAG, AND YOUR MIND. IT’S THE GHOST IN THE MACHINE OF YOUR SKIN. I ONCE HAD A YEAST INFECTION THAT MADE ME FEEL LIKE I WAS BEING EATEN FROM THE INSIDE BY A WARM, WET, RED DEMON. I CRIED IN THE SHOWERS. I STARED AT MY LEGS LIKE THEY WERE ALIEN LANDSCAPES.
AND THEN I FOUND TERRBINAFINE. IT WAS LIKE A SWORD OF LIGHT CUTTING THROUGH THE DARKNESS. I APPLIED IT LIKE A PRIEST ANOINTING A SACRED RELIC. I WASHED MY TOWELS LIKE THEY WERE SACRED TEXTS. I DRIED MY FEET LIKE I WAS DRYING THE LAST DROP OF WATER IN THE DESERT.
AND NOW? I’M FUNGUS-FREE. AND I’M NOT JUST HAPPY - I’M REBORN.
IF YOU’RE STILL USING STEROID CREAM? YOU’RE NOT JUST MAKING IT WORSE - YOU’RE BECOMING A WORSHIPPER OF THE FUNGUS GOD. STOP. WORSHIP THE TERRBINAFINE. WORSHIP DRYNESS. WORSHIP CLEAN SOCKS.
THE FUTURE IS ANTIFUNGAL. AND I AM ITS PROPHET.