Introduction to Naturopathic Medicine for Pancreatic Duct Blockage
As a blogger passionate about naturopathic medicine, I have always been fascinated by the various ways in which this holistic approach can help treat numerous ailments. One such condition that can be effectively managed by naturopathic medicine is pancreatic duct blockage. In this article, we will explore the role of naturopathic medicine in treating this condition, and how it can provide relief to those suffering from it.
Understanding Pancreatic Duct Blockage
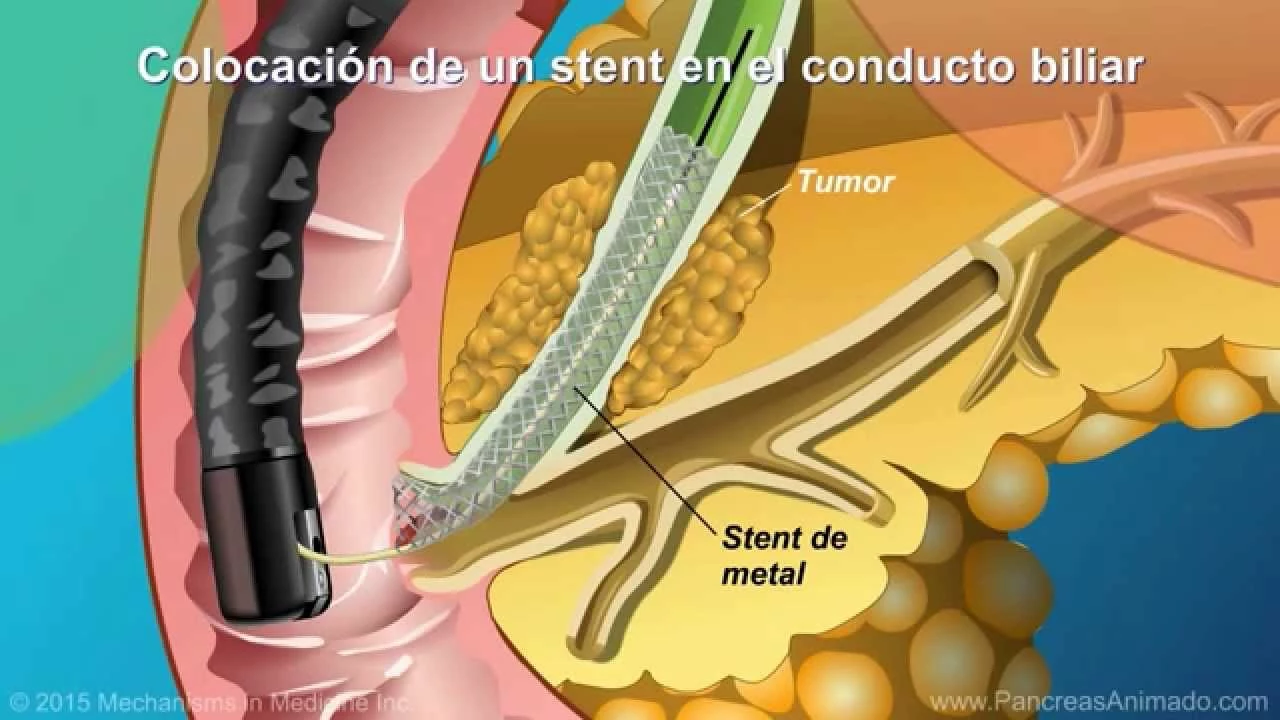
Before diving into the naturopathic treatments, it is essential to understand what pancreatic duct blockage is and how it affects the body. The pancreas is a vital organ that plays a crucial role in digestion and blood sugar regulation. It secretes digestive enzymes and hormones such as insulin and glucagon. Pancreatic duct blockage occurs when the ducts that carry these enzymes and hormones become obstructed, resulting in inflammation and other complications. Some common causes of pancreatic duct blockage include gallstones, tumors, and chronic pancreatitis.
Naturopathic Approach to Diagnosis
A naturopathic doctor will begin by conducting a thorough assessment of the patient's medical history, lifestyle, dietary habits, and overall health. This comprehensive evaluation enables the practitioner to identify any underlying causes or contributing factors that may be leading to the pancreatic duct blockage. They may also recommend specific diagnostic tests, such as imaging studies or blood tests, to confirm the diagnosis and assess the severity of the condition.
Dietary Modifications for Pancreatic Duct Blockage
One of the primary naturopathic treatments for pancreatic duct blockage involves making dietary changes to support optimal pancreatic function. A naturopath will recommend a diet that is low in fat and high in fiber, as this can help reduce the risk of gallstones, one of the leading causes of blockage. Additionally, they may recommend consuming more anti-inflammatory foods, such as fruits, vegetables, and whole grains, to help reduce inflammation and promote overall digestive health.
Supplements to Support Pancreatic Health
Along with dietary changes, a naturopath may suggest specific supplements to support pancreatic function and overall digestive health. These may include digestive enzymes, probiotics, and certain vitamins and minerals, such as vitamin D, magnesium, and selenium. It is essential to speak with a qualified naturopathic practitioner before starting any supplement regimen to ensure that it is safe and appropriate for your specific needs.
Herbal Remedies for Pancreatic Duct Blockage
Naturopathic medicine also incorporates the use of herbal remedies to address specific health concerns, including pancreatic duct blockage. Some herbs that may be beneficial in this context include milk thistle, turmeric, and ginger, which have anti-inflammatory and antioxidant properties. A naturopathic doctor will customize an herbal treatment plan based on the individual needs and health goals of the patient.
Stress Management and Lifestyle Changes
Stress is known to exacerbate many health conditions, and pancreatic duct blockage is no exception. Naturopathic doctors recognize the importance of addressing stress and its impact on overall health. They may recommend various stress management techniques, such as meditation, yoga, or deep breathing exercises, to help reduce stress levels and promote overall well-being. Additionally, they may suggest other lifestyle changes, such as regular exercise and adequate sleep, to support optimal health and healing.
Acupuncture for Pancreatic Duct Blockage
Acupuncture is another naturopathic treatment that can help alleviate symptoms associated with pancreatic duct blockage. This ancient Chinese medicine technique involves the insertion of thin needles at specific points on the body to stimulate the flow of energy, or qi. Acupuncture has been shown to help reduce inflammation, alleviate pain, and improve digestive function, making it a valuable treatment option for individuals with pancreatic duct blockage.
Conclusion: The Benefits of Naturopathic Medicine for Pancreatic Duct Blockage
In conclusion, naturopathic medicine offers a holistic and individualized approach to treating pancreatic duct blockage. By addressing the root causes of the condition and promoting overall health through dietary modifications, supplements, herbal remedies, stress management, and acupuncture, naturopathic medicine can provide relief to those suffering from pancreatic duct blockage. If you or a loved one is struggling with this condition, consider consulting with a naturopathic doctor to explore the potential benefits of this natural and comprehensive approach to healing.
Reading about the role of naturopathic medicine in pancreatic duct blockage feels like stepping onto a stage where every organ is a character craving a curtain call of relief. First, imagine the pancreas as a weary performer, its ducts clogged like backstage doors jammed shut. A naturopathic practitioner steps in like a seasoned director, rewriting the script with dietary modifications that low the fat and raise the fiber, allowing the scene to unfold with smoother digestion.
Then comes the supporting cast of anti‑inflammatory foods-vibrant vegetables, crisp fruits, whole grains-each delivering a line of antioxidants that soothe the inflamed backdrop. Supplements such as digestive enzymes, probiotics, and the mineral trio of magnesium, selenium, and vitamin D take their cue, bolstering the protagonist’s strength.
Herbal allies-milk thistle, turmeric, ginger-enter with flourish, their phytochemicals acting as understudies that quell oxidative stress. Stress management techniques like meditation and yoga become the quiet intermission, giving the body a moment to reset its rhythm.
Acupuncture needles, like precise spotlights, illuminate meridian pathways, urging the qi to flow and the pancreas to perform its duties without obstruction. Throughout this holistic production, the practitioner tailors each element to the individual, ensuring that the audience of cells and enzymes receives a personalized encore.
The result? A symphony of natural interventions that, when harmonized, can lift the veil of blockage and restore the pancreas to its rightful role on the health stage. This is not a quick fix but an ongoing rehearsal of lifestyle, nutrition, and mind‑body balance, all choreographed to support lasting wellness.
While the prose paints a romantic tableau, the underlying methodology remains entrenched in pseudoscientific dogma, lacking rigorous randomized controlled trials to substantiate any claimed efficacy. The reliance on anecdotal evidence and herbal amalgams contravenes evidence‑based standards, rendering the approach scientifically untenable. Moreover, the invocation of "energy" and "qi" betrays a departure from physiological plausibility, substituting metaphysical constructs for measurable biomarkers. The dietary recommendations, though ostensibly low‑fat, ignore macronutrient balance and fail to address the pathophysiology of lithogenic bile formation. Supplement regimens, particularly exogenous enzymes, are presented without dosage justification or pharmacokinetic data, potentially engendering adverse interactions. In sum, the article promulgates a narrative that conflates holistic rhetoric with clinical effectiveness, an intellectually dishonest synthesis that warrants skeptical scrutiny.
Permit me to elucidate that the discourse presented suffers from an egregious paucity of mechanistic clarity; one must appreciate that pancreatic duct obstruction is fundamentally a consequence of calculi formation, neoplastic encroachment, or chronic inflammatory remodeling. The proposition that merely augmenting fiber intake will dissolve biliary calculi is, to put it mildly, a misapprehension of lithogenesis. Furthermore, the suggested phytotherapeutics-milk thistle, turmeric, ginger-though rich in polyphenols, lack validated bioavailability profiles sufficient to exert clinically relevant anti‑inflammatory action within the pancreatic microenvironment. The author's omission of enzymatic pathophysiology, particularly the role of secretin and cholecystokinin, betrays a superficial engagement with the endocrine dimension of the organ. In light of these considerations, a more rigorous, interdisciplinary approach-integrating gastroenterological assessment, imaging, and evidence‑based pharmacotherapy-remains indispensable.
This whole naturopathic hype is just a scam.
Wow you really think that whole thing is a scam, but it's cool to see the different views. I guess everyone has their own thing, so we all just chill and see what works.
The discussion invites a contemplation of health as an integrated phenomenology, wherein the corporeal and psychosomatic realms intersect. One might argue that the epistemic value of holistic interventions lies not merely in biochemical modulation but in the cultivated awareness of bodily signals. From a philosophical stance, such practices embody a form of lived ontology, encouraging individuals to navigate their constitutive narratives of wellness. While empirical validation remains a prudent pursuit, the experiential dimension should not be dismissed outright as frivolous.
Our indigenous healing traditions have championed natural remedies long before Western quacks tried to appropriate them; the claim that naturopathy is some novel miracle is a blatant insult to the cultural heritage of nations that have safeguarded health through centuries of empirical wisdom.
Respecting the profound legacy of traditional medicine necessitates a balanced discourse that neither dismisses modern scientific rigor nor vilifies ancestral practices. While the fervor expressed underscores legitimate concerns about cultural appropriation, constructive dialogue should aim to harmonize validated therapeutic modalities with time‑honored knowledge, fostering a collaborative paradigm for patient-centered care.