Oral Medication Effectiveness: What Really Works and Why It Matters
When you swallow a pill, it doesn’t just magically work. Oral medication effectiveness, how well a drug performs after being taken by mouth. Also known as oral bioavailability, it’s the real measure of whether your treatment actually reaches your bloodstream at the right level to help. Many people assume if a drug is prescribed, it’s guaranteed to work—but that’s not true. Factors like stomach acid, food timing, gut health, and even how fast your body breaks it down can cut effectiveness in half. You might be taking the right medicine, but if your body can’t absorb it, you’re wasting time and money.
That’s why bioavailability, the percentage of a drug that enters circulation after oral intake matters more than dose size. Two people taking the same 50mg pill might get totally different results—one gets full benefit, the other feels nothing. This isn’t about willpower or compliance—it’s biology. Some drugs need an empty stomach. Others need fat to dissolve. Some are destroyed by stomach acid unless they’re coated. And if you’re on multiple meds, interactions can block absorption. For example, antacids can stop antibiotics from working. Iron supplements can tie up thyroid meds. These aren’t rare edge cases—they show up in hospital formularies, pharmacy alerts, and real-world adherence studies.
Then there’s medication adherence, how consistently patients take their drugs as directed. Even the most effective oral medication fails if you skip doses, forget to take it at the same time, or stop early because you feel better. This isn’t just about memory—it’s about side effects, cost, complexity, and trust. If your pill makes you dizzy, costs too much, or comes with confusing instructions, you’re less likely to stick with it. That’s why tools like pill organizers, reminder apps, and clear labeling aren’t luxuries—they’re part of the treatment plan. And when adherence drops, so does effectiveness. It’s a cycle: poor absorption leads to no results, which leads to distrust, which leads to skipping doses, which leads to worse outcomes.
And let’s not forget side effects, unwanted reactions that can force people to stop taking meds. Sometimes, the side effect isn’t just annoying—it’s dangerous. Opioid-induced adrenal insufficiency, for example, doesn’t show up right away. It creeps in over months, and when you get sick or stressed, your body can’t respond. That’s not a side effect you can ignore. Other drugs, like statins or antibiotics, have delayed reactions that confuse patients. If you don’t know when to expect a reaction, you might think the drug isn’t working—or worse, you might blame yourself.
What you’ll find below isn’t just a list of articles. It’s a practical guide to understanding why your pills work—or don’t. From how generics are chosen in hospitals to why some drugs need to be taken with food, from interpreting pharmacy alerts to knowing when a supplement interferes with your meds—every post here answers real questions people face daily. No fluff. No theory without practice. Just what you need to make sure your oral medications actually do what they’re meant to.
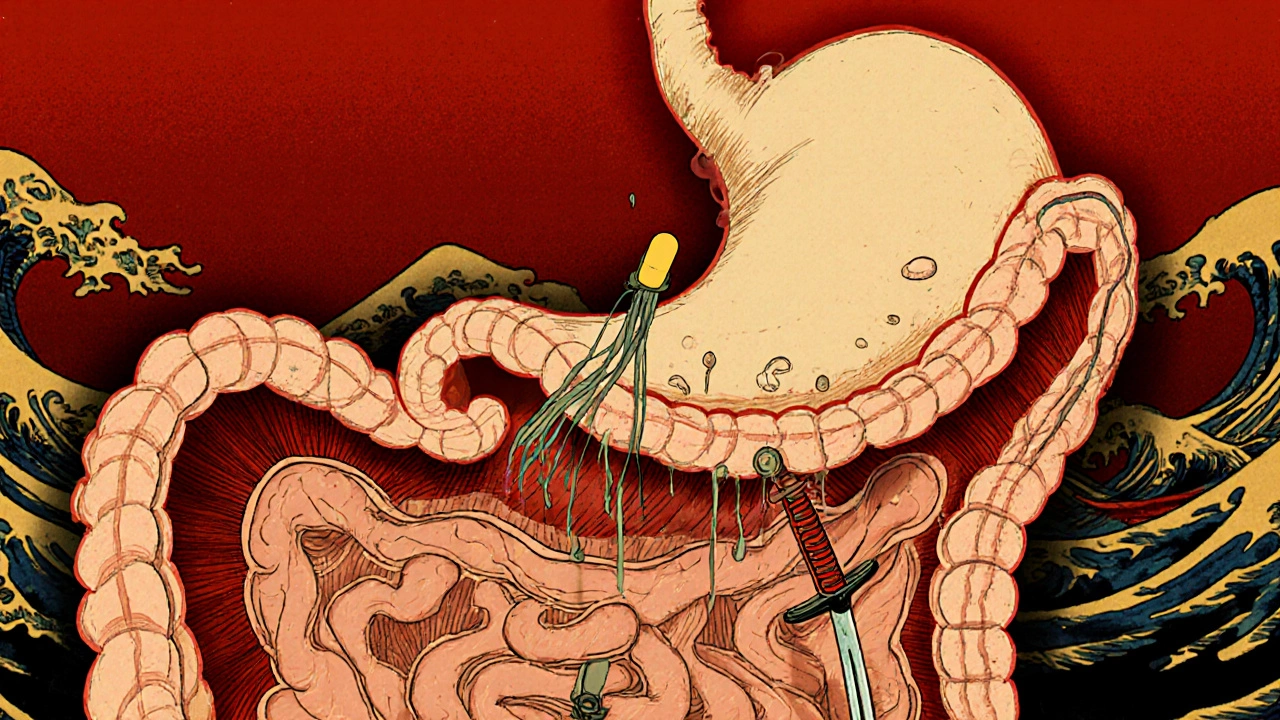
Gastrointestinal Medications: Why Absorption Issues Ruin Effectiveness
Many gastrointestinal medications fail to work because of absorption issues caused by gut physiology, food interactions, and disease. Learn why your pills might not be working and what you can do about it.
read more