
Getting a generic drug approved isn’t just about copying a pill. When the drug is complex-like an inhaler, a topical cream, or a liposomal injection-proving it works the same as the brand-name version becomes a scientific marathon. The goal is simple: make sure patients get the same safety and effectiveness at a lower cost. But the path to proving that? It’s anything but simple.
What Makes a Generic Drug "Complex"?
Not all generics are created equal. The FDA defines complex generics as products where the drug’s structure, delivery method, or formulation makes it hard to show it behaves the same way in the body as the original. These aren’t your typical tablets or capsules. They include:- Liposomes and nanoparticles that trap drugs inside tiny fat bubbles
- Inhalers that spray medicine deep into the lungs
- Topical gels and creams meant to act on the skin, not enter the bloodstream
- Extended-release injectables that release medicine slowly over weeks
- Drug-device combos like auto-injectors or nasal sprayers
These aren’t just harder to make. They’re harder to measure. Traditional bioequivalence studies rely on blood samples to track how much drug gets into circulation. But if the drug is supposed to stay on the skin or act in the lungs, blood levels tell you nothing. That’s where things get messy.
The Bioequivalence Problem: Blood Tests Don’t Work Here
For a regular pill, bioequivalence means showing that the generic delivers the same amount of drug into the blood at the same speed as the brand. The FDA requires the 90% confidence interval for two key numbers-AUC (total exposure) and Cmax (peak concentration)-to fall between 80% and 125% of the brand’s values. That’s a clear, measurable standard.Now imagine a corticosteroid cream for eczema. The drug isn’t meant to enter the blood. It’s meant to sit on the skin and reduce inflammation. Measuring blood levels? Useless. The real question is: how much drug actually penetrates the top layers of skin? And how consistently? There’s no agreed-upon test for that. Manufacturers have to guess, build prototypes, test them on volunteers, and hope their method satisfies regulators.
The same problem hits inhalers. A generic asthma inhaler must deliver the same particle size, spray pattern, and lung deposition as the brand. But how do you prove that? You can’t stick a sensor in someone’s lungs. You rely on surrogate tests-like measuring how much drug lands on a filter or how fast it sprays. But these don’t always predict what happens inside the body. And different countries accept different tests. The FDA might accept one method. The EMA might demand another. That means companies have to run two separate development programs just to get approval in both markets.
Manufacturing Is a Minefield
Complex generics often have more than 10 ingredients. Each one matters. A tiny change in the type of emulsifier in a cream, the particle size of the active ingredient, or the pressure used to fill an inhaler can change how the drug performs. These aren’t just minor tweaks-they can alter the whole behavior of the product.Take liposomal doxorubicin, a cancer drug. The drug is wrapped in a fatty shell. If the shell is too thick, the drug doesn’t release properly. Too thin, and it leaks out too fast. The manufacturing process-how the liposomes are formed, purified, and sterilized-has to be perfect. Even small shifts in temperature or mixing speed during production can ruin batch consistency. And unlike a simple tablet, you can’t just test one batch and assume the next will be the same. Every batch needs full characterization.
That’s why 76% of generic manufacturers say stability testing is a top challenge. These products degrade faster. Heat, humidity, light-they all attack complex formulations. A cream that works today might fail in six months if the preservative isn’t just right. And since you can’t always measure the drug’s effect directly, you’re left guessing whether stability changes will impact performance.
The Secret Recipe Problem
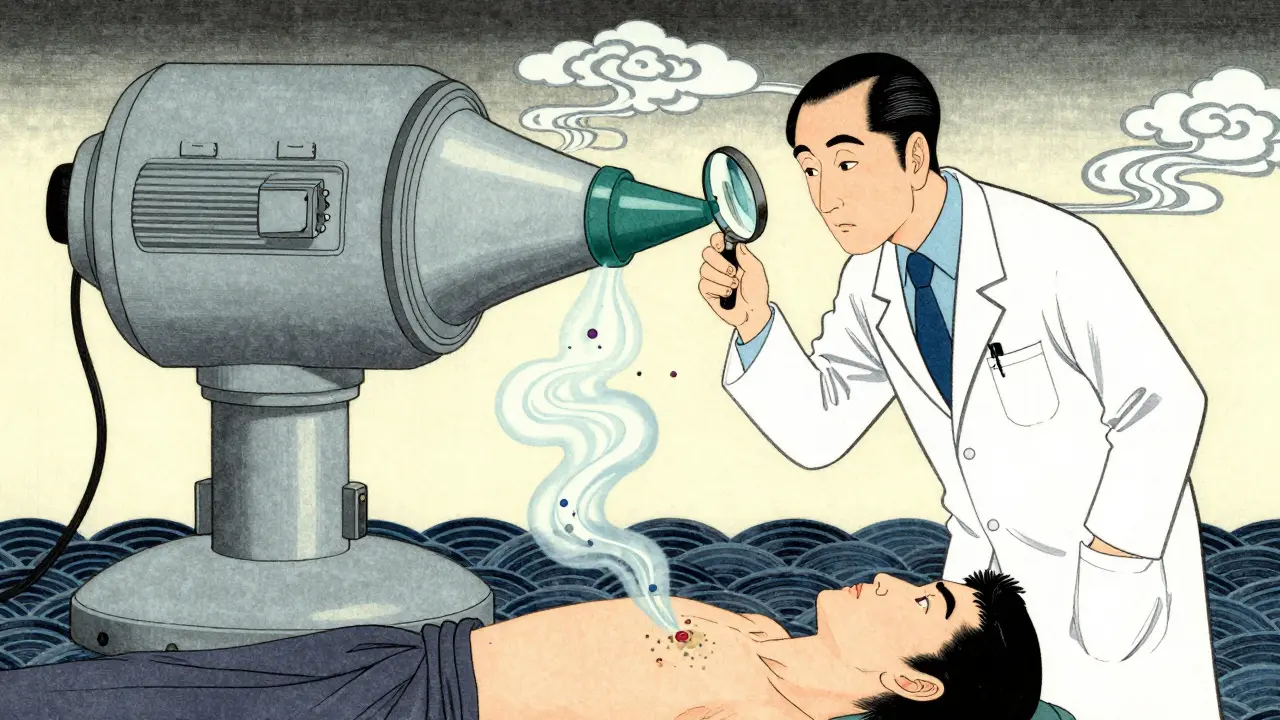
Here’s the cruel twist: generic makers have to reverse-engineer the brand-name drug without knowing its formula. They don’t get the recipe. They don’t know which excipients were chosen, why, or how they were processed. They have to figure it out by analyzing the product-like a detective trying to recreate a cake from a single bite.This is called de-formulation. It takes years. Teams of chemists and engineers spend months breaking down the product, testing components, and rebuilding it. Even then, they might miss something. A tiny amount of a stabilizer, a specific crystalline form of the active ingredient, or a hidden manufacturing step-these can be the difference between approval and rejection.
One company spent three years trying to match a topical testosterone gel. They got the active ingredient right. They matched the viscosity. But the drug didn’t absorb the same way. Turns out, the brand used a specific grade of alcohol that altered skin penetration. No one had documented that detail. The generic failed three bioequivalence studies before they figured it out.
Regulators Are Trying to Help-But It’s Not Enough
The FDA knows this is a problem. That’s why they created the Complex Generic Drug Products Committee. They’ve published 15 new guidance documents since 2022 for products like inhaled budesonide, topical corticosteroids, and transdermal patches. They’re pushing for Quality by Design-planning for stability and performance from day one, not after the product fails.They’re also investing in new tools. Instead of relying only on blood tests, they’re developing:
- Imaging techniques to track drug movement through skin
- Computer models that simulate how particles behave in the lungs
- Physiologically-based pharmacokinetic (PBPK) models that predict drug behavior based on chemistry and biology
PBPK modeling is a game-changer. It could cut bioequivalence study needs by 40-60% for some products. Instead of running 50 human trials, you might run five, plus detailed lab tests. But regulators still need to agree on when these models are good enough. And right now, they’re not widely accepted.
Companies that engage the FDA early-before they spend millions-have a 35% higher chance of approval. But many small manufacturers can’t afford the time or cost of those early meetings. So they guess, build, test, and fail.

The Cost of Failure
Developing a complex generic takes 2.5 to 3 times longer than a regular one. It costs 3-5 times more. And failure rates? Over 70% at the bioequivalence stage.That’s why only 10-15% of complex generic applications get approved, compared to over 80% for simple generics. There are around 400 complex brand-name drugs on the market with no generic alternatives. That’s a $120 billion gap.
And it’s not just about money. Patients suffer. A patient on an expensive inhaler might skip doses because they can’t afford it. A cancer patient stuck with a costly liposomal drug might delay treatment. The whole point of generics is to make medicine accessible. But for complex drugs, that promise is still out of reach for most.
What’s Next?
The future isn’t hopeless. Industry and academic groups like the Center for Research on Complex Generics are creating standardized testing methods. Twelve new protocols for liposomes, nanosuspensions, and inhalers were published in 2022-2023. The ICH is working on global standards for impurities in complex products, expected to finalize in late 2024.Market forecasts show complex generic sales growing from $15 billion in 2023 to $45 billion by 2028. That’s a 24.6% annual growth rate. The pressure to cut costs in specialty medicine is too strong to ignore.
But progress depends on three things: better tools, clearer regulations, and more collaboration. Manufacturers need to work with regulators early. Regulators need to accept new science, not just old methods. And everyone needs to stop treating complex generics like simple pills.
The science is advancing. The demand is growing. The question isn’t whether complex generics will become common-it’s how fast we can make the system catch up.
This is why pharma is a joke. They charge $1000 for a pill that costs $2 to make, then act shocked when generics can't replicate it. It's not science, it's a monopoly game. And don't even get me started on how they patent the *container* now. 🤡
The core issue is lack of analytical standardization for non-systemic delivery systems. Blood PK is obsolete for topical inhaled and liposomal. We need in vivo imaging PBPK and microdialysis models validated across jurisdictions. EMA FDA and PMDA are still stuck in 2005 thinking. No wonder approval rates are abysmal
I had no idea how hard this was 😅 I thought generics were just cheaper versions but wow this is insane. Like trying to copy a cake by tasting one bite and guessing the oven temp. Big respect to the scientists trying to figure this out. We need more funding for this stuff 💪
They don't want generics to work. That's why the tests are impossible. The same people who profit off brand drugs are the ones writing the rules. PBPK models? Sure... but only if they're *their* models. Watch how fast the FDA changes its mind when a big pharma exec shows up. This is all about control. Not science.
The real tragedy here is patients who can't afford their meds and don't understand why there's no cheaper option. I've seen people skip insulin doses because they can't afford the brand and the generic isn't approved yet. We need to stop treating complex generics like they're just pills. They're delivery systems. They need different rules. And regulators need to stop being scared of new tech and start being scared of patients dying because of bureaucracy
This whole thing is a mess and everyone knows it. The FDA spends millions on studies that go nowhere because they won't accept new methods. Meanwhile small companies go broke trying to reverse-engineer a cream that took Big Pharma 15 years and $200M to develop. Someone needs to cut the red tape. We don't need 50 human trials for a topical gel. We need smart science not old school bureaucracy
I can't believe we're still letting corporations get away with this. They patent the *fatty shell* around a drug. That's not innovation. That's theft. And regulators are complicit. If you can't prove bioequivalence because the system is rigged, then the whole approval process is a scam. Patients are paying for corporate greed and the FDA is the enforcer. Wake up people
This is why I love science 😭 The fact that people are trying to solve this with imaging and computer models? So cool. I wish more people knew how hard this stuff is. It's not just 'make a copy' it's like recreating a symphony from one note. Hats off to the teams doing this. 🙌
The notion that PBPK modeling can replace human trials is scientifically unsound. Variability in human physiology cannot be fully captured by computational models. Regulatory reliance on such methods without extensive validation risks patient safety. The current framework, while imperfect, is grounded in empirical evidence. We must not sacrifice rigor for convenience.