Most people who lose weight gain it back. Not because they lack willpower, but because they never fixed the thinking that led them to overeat in the first place. If you’ve tried diets that left you hungry, frustrated, or guilty after one slip-up, you’re not broken. You’re just working with outdated tools. Behavioral weight loss therapy, especially when it uses cognitive behavioral therapy (CBT), doesn’t just tell you what to eat. It rewires how you think about food, your body, and failure.
Why Diets Fail and CBT Works
Diets focus on calories, portions, and rules. CBT focuses on the voice in your head that says, "I blew it, so I might as well eat the whole cake." That voice isn’t weak-it’s learned. And learned patterns can be unlearned.
Research shows CBT for weight loss isn’t magic. It’s methodical. A 2023 meta-analysis of 9 studies with over 900 people found those using CBT lost an average of 1.6 BMI points more than those on standard diet plans. That’s not dramatic, but it’s real-and more importantly, it lasts longer because it changes how you respond to stress, boredom, or emotional triggers.
Standard behavioral programs teach you to log meals and walk 10,000 steps. CBT teaches you why you reach for snacks when you’re anxious, why you think one cookie means you’ve failed, and how to stop that cycle before it starts.
The 6 Cognitive Strategies That Actually Change Behavior
Not all CBT is the same. The most effective weight loss programs use six core cognitive tools, backed by years of clinical testing.
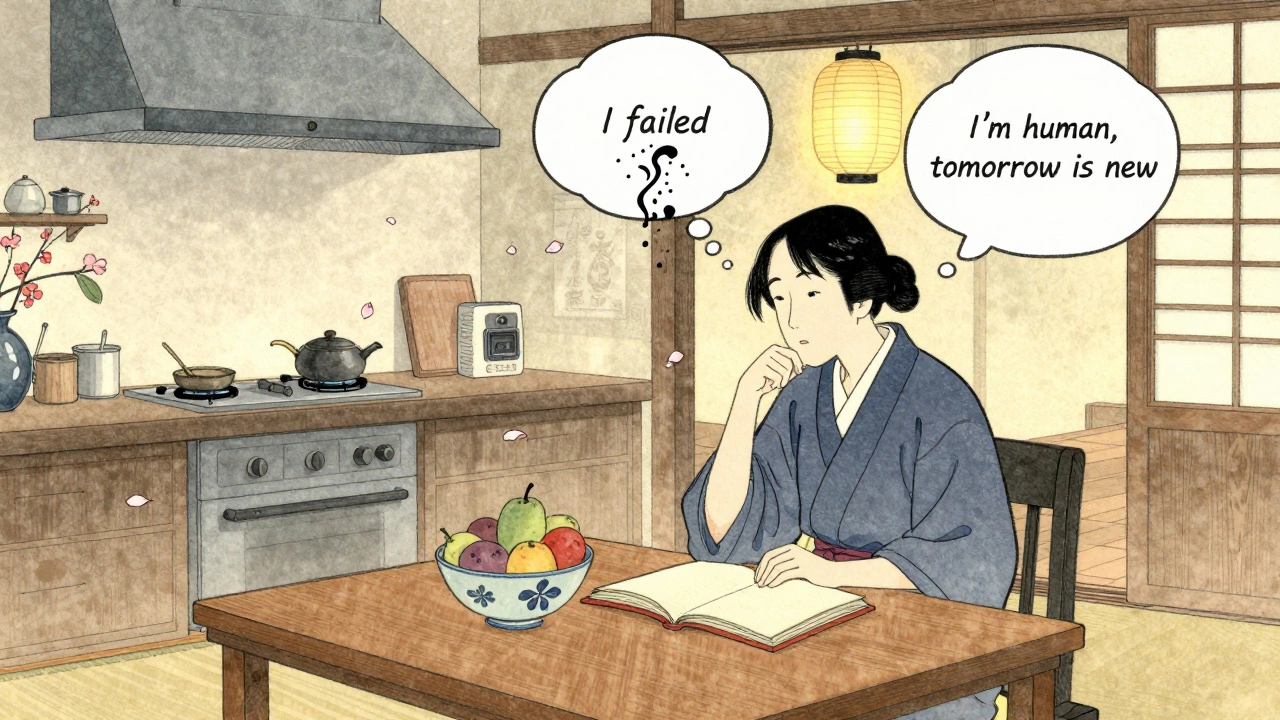
- Cognitive Restructuring: This is the heart of CBT. It’s about catching thoughts like, "I’ll never be thin," or "I can’t trust myself around food," and replacing them with facts. For example: "I had a tough day and ate more than planned. That doesn’t mean I’m a failure-it means I’m human. Tomorrow is a new day." Studies show people who practice this reduce emotional eating by 63%.
- Self-Monitoring: Writing down what you eat and how you feel isn’t just about accountability. It’s about awareness. People who track their food and moods consistently lose 5-10% more weight than those who don’t. You don’t need a fancy app. A notebook works. The key is writing it down immediately-not remembering it later.
- Stimulus Control: Your environment is your biggest trigger. If your kitchen is full of snacks, your brain learns to associate that space with eating. CBT helps you change the setup: keep junk food out of sight, store healthy snacks at eye level, avoid eating in front of the TV. Simple changes, big results.
- Goal Setting: Vague goals like "lose weight" fail. SMART goals work: Specific, Measurable, Achievable, Relevant, Time-bound. Instead of "I’ll eat healthier," try "I’ll have a vegetable with dinner every night this week." Small wins build confidence.
- Problem-Solving for High-Risk Situations: What do you do when you’re invited to a party with no healthy options? When you’re stressed and your partner is away? CBT doesn’t just prepare you for perfect days-it prepares you for messy ones. You role-play scenarios. You plan alternatives. You build a backup plan before you need it.
- Relapse Prevention: This isn’t about avoiding mistakes. It’s about knowing what to do when you make them. CBT teaches you that one off-day doesn’t erase progress. It’s a data point, not a disaster. People who learn this are 40% less likely to quit their program.
CBT vs. Other Weight Loss Methods
How does CBT stack up against other approaches?
| Approach | Average Weight Loss (6 months) | Long-Term Retention (2 years) | Psychological Benefits |
|---|---|---|---|
| Standard Diet & Exercise | 5.1% | 15-20% | Minimal |
| CBT Alone | 8.2% | 20-30% | 40% reduction in anxiety/depression |
| CBT + Motivational Interviewing | 12.7% | 35-40% | Significant improvement in self-efficacy |
| Digital Apps (Noom, WW) | 3.2% | 10-15% | Moderate, limited by lack of human support |
CBT doesn’t just help you lose weight-it helps you feel better while doing it. People report less guilt, less shame, and more control over their choices. That’s why CBT is now recommended as a first-line treatment by the American Heart Association.

Who Benefits Most from CBT for Weight Loss?
CBT isn’t for everyone-but it’s especially powerful for certain groups.
- People with binge eating disorder (BED): Over half of BED patients no longer meet diagnostic criteria five years after CBT, according to a 2016 study. That’s not just weight loss-it’s recovery.
- Those who’ve tried diets before: If you’ve lost weight and regained it, CBT helps you understand why. It breaks the cycle of restriction and rebound.
- People with depression or anxiety: Weight and mood are deeply linked. CBT tackles both at once. Studies show 40% fewer symptoms of depression after CBT-based weight programs.
- Those who feel stuck emotionally: If you eat because you’re bored, lonely, or overwhelmed, CBT gives you other tools to cope.
What’s Missing from CBT? The Real Limitations
CBT isn’t a cure-all. And pretending it is sets people up for disappointment.
Most people regain 30-35% of lost weight within the first year-even with CBT. Why? Because weight regulation is biological, not just psychological. Hormones, metabolism, genetics-they all play a role.
Another problem: access. There’s only one certified CBT obesity specialist for every 125,000 eligible patients in the U.S. Therapy costs money. Insurance often covers only 12 sessions, even though studies show 20+ sessions yield 27% better results.
And let’s be honest: CBT takes effort. It’s not a quick fix. It takes 8-12 weeks to get good at identifying distorted thoughts. Many people quit before they see results.

How to Get Started with CBT for Weight Loss
You don’t need a therapist to start using CBT tools-but you do need structure.
- Start a thought journal. For one week, write down: What happened? What did you think? What did you feel? What did you do? Look for patterns. Do you always eat after an argument? After scrolling social media?
- Challenge one distorted thought. Pick the most common negative thought you have about food or your body. Write down evidence for and against it. Replace it with a balanced one. Example: "I can’t eat carbs" → "I can eat carbs in moderation without losing control."
- Change one environmental trigger. Remove one snack from your kitchen. Keep fruit on the counter. Move the TV remote so you have to stand up to change the channel.
- Set one small, specific goal. "I’ll drink water before every meal." Not "I’ll eat better."
- Plan for setbacks. What will you do if you eat a whole pizza? Write your response now: "I’ll acknowledge it, learn from it, and move on. One meal doesn’t define me."
The Future: CBT Isn’t Going Away-It’s Evolving
Even with new weight-loss drugs like semaglutide, experts agree: the psychological piece is non-negotiable. The NIH is now funding $14.7 million in research to combine CBT with GLP-1 medications. Why? Because drugs help you lose weight. CBT helps you keep it off.
Group CBT is becoming more popular-cheaper, just as effective, and less isolating. Online programs like Noom and WeightWatchers Beyond the Scale use CBT principles, but they can’t replace the human connection. Studies show therapist-led CBT leads to nearly double the weight loss of apps alone.
What’s clear? The future of weight loss isn’t about the next miracle diet. It’s about building a mindset that can handle real life-messy, stressful, imperfect life. CBT gives you the tools to do that.
Can I do CBT for weight loss on my own?
Yes, but it’s harder. You can use workbooks, apps, or online courses that teach CBT principles. Many people start this way. But research shows the best results come from working with a trained therapist, especially in the early stages. If you’re struggling with binge eating, depression, or have tried diets repeatedly, professional guidance makes a big difference.
How long does CBT for weight loss take?
Most programs last 12 to 26 weeks, with weekly sessions. You’ll start noticing changes in your thinking after 4-6 weeks. But mastering cognitive skills takes time-often 8-12 weeks. The most successful people stick with it for at least 6 months, even after reaching their goal weight, to build lasting habits.
Does CBT work for people who’ve had bariatric surgery?
Absolutely. Surgery changes your stomach, but not your relationship with food. Many people regain weight after surgery because old thought patterns return. CBT helps them adjust to new eating habits, manage emotional triggers, and avoid using food as comfort. Studies show patients who get CBT after surgery are 40% more likely to maintain long-term weight loss.
Is CBT covered by insurance?
Sometimes. In the U.S., only about 32% of insurance plans cover more than 12 sessions of CBT for weight loss. Coverage varies by state and provider. Some employers offer wellness programs that include mental health support for weight management. Always ask your insurer about "behavioral health services for obesity"-that’s the key phrase to use.
What if I don’t have time for therapy?
Start small. You don’t need 50-minute sessions to begin. Try a 10-minute daily journal. Challenge one negative thought each day. Change one habit in your kitchen. These are all CBT tools. Progress doesn’t require hours-it requires consistency. Even 15 minutes a day, five days a week, can shift your mindset over time.
Diets are just capitalism selling you hope. CBT? Same thing with more jargon. I ate a cookie once and felt guilty for a week. Then I just stopped caring. Life’s too short to overthink snacks.
I love this breakdown. Seriously. I tried every diet under the sun-keto, intermittent fasting, cabbage soup-and I’d bounce back harder each time. Then I started journaling my thoughts before I ate. Turns out, I wasn’t hungry-I was lonely. Changed my whole life. Not just my weight. I’m not ‘fixing’ myself anymore. I’m just learning how to be kinder to myself. Thank you for writing this.
While the empirical evidence supporting cognitive behavioral therapy in the context of weight management is indeed compelling, one must also acknowledge the structural limitations inherent in its accessibility. The disparity between demand and availability of certified practitioners remains a significant barrier for the majority of the population. Furthermore, the socioeconomic stratification of healthcare access renders such interventions inequitable in practice, despite their theoretical efficacy.
It’s not about food. It’s about the existential void we try to fill with carbs. CBT just gives you a fancy word for ‘stop using pizza as a therapist.’
This is the first time I’ve read something about weight loss that didn’t make me feel like a failure. I’ve been stuck in this cycle for years. I started writing down my thoughts after a bad day-just one line. And now? I don’t eat the whole bag of chips anymore. I just sit with the feeling. It’s small. But it’s mine. Thank you.
The data presented here is methodologically sound and aligns with peer-reviewed literature on CBT efficacy in behavioral weight management. However, the omission of long-term neurobiological correlates-such as changes in dopamine receptor sensitivity post-intervention-is a notable limitation in the discussion of sustained outcomes.
CBT? LOL. Big Pharma and insurance companies love this. They don't want you cured-they want you *managed*. They know if you fix your brain, you won't need their drugs or their endless ‘programs.’ This is just another trap. Watch your thoughts… or watch your wallet. 😏
It’s fascinating how we’ve turned survival into a moral failing. We’re wired to seek calories-evolution didn’t care about BMI charts. CBT doesn’t change biology; it just gives us a language to stop hating ourselves for being human. Maybe that’s the real win.
You don’t need to be perfect. You just need to show up. One journal entry. One snack moved. One thought challenged. That’s enough. I’ve been where you are. You’re not behind. You’re just beginning.
Western medicine is so weak. In India, we don’t need therapy to eat less-we have discipline. We have culture. We have family. You people think food is a psychological problem? No. It’s a lack of willpower. CBT is just an excuse for laziness.
Let’s be precise: the meta-analysis cited (2023) had a pooled effect size of d = 0.48 for BMI reduction, which is moderate-not ‘dramatic’ as claimed. Moreover, the attrition rate in CBT trials hovers around 40%, suggesting that while effective for responders, it’s not universally applicable. Also, ‘SMART goals’? Please. That’s management-speak from 1981. We’ve moved beyond acronyms.
cbt? sounds like therapy for people who cant spell ‘diet’ right 😂 i just eat less. its not that hard. why do we need 6 strategies for this?
Of course it works. People who can afford therapists and have time to journal are already privileged. Meanwhile, single moms working two jobs and eating gas station food are just ‘not trying hard enough.’ CBT is a luxury. And you’re selling it like it’s salvation.
What if the real problem isn’t the thoughts… but the world? Why are we expected to ‘manage’ our emotions in a system that gives us no time, no safety net, and no real food? CBT helps us cope-but what if we needed to change the system instead of just our minds?
Just wanted to say: if you’re reading this and thinking, ‘I can’t afford therapy,’ start with the thought journal. Use a sticky note. Use your phone notes. One sentence a day. ‘I felt sad. I ate chips. I didn’t regret it.’ That’s CBT. No degree needed. You’re already doing it. Keep going.
Wow. I didn’t expect this to hit so hard. I tried CBT once, quit after two weeks because I thought I was ‘failing’ at it. Then I read your comment about it being about kindness, not perfection. I started again yesterday. Just one thought. Just one day. I think… I think I’m ready to stop fighting myself.